Traditional landmarked-based wrist aspirations are difficult and often unsuccessful. Even in the hands of experienced rheumatologists who perform frequent radiocarpal aspirations and injections, landmark-based aspirations in joints throughout the body can be missed more than 60 percent of the time.1
Fortunately, for emergency physicians, the use of point-of-care ultrasound for anatomical visualization allows for easy detection and localization of wrist effusions and for reliable joint aspiration.2 Ultrasound not only makes this procedure easier to perform but should decrease the likelihood of iatrogenic tendon injury.
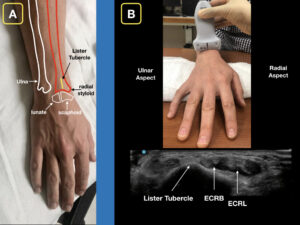
Figure 1A: The dorsal aspect of the distal forearm and radiocarpal joint. Note Lister’s tubercle and its relation to the scaphoid bone. Figure 1B: A roll is placed on the palmar aspect of the wrist for slight flexion. With the ultrasound probe in a transverse orientation, slide distally until Lister’s tubercle is visualized. The extensor carpi radialis brevis tendon (ECRB) and extensor carpi radialis longus (ECRL) can be seen on the radial aspect of Lister’s tubercle. Credit: Arun Nagdev
The radiocarpal joint is composed primarily of the distal radius as it articulates with the scaphoid and lunate bones (see Figure 1A). This can be palpated on the unaffected side but can be difficult to identify by landmarks in many patients, especially with a marked swelling from an inflammatory or infectious process.
Our technique provides an easy-to-obtain ultrasonographic view and reliable method to evaluate the radiocarpal joint and perform an aspiration if needed. We have successfully used this method to rule in and rule out septic arthritis in multiple cases, allowing our clinicians to develop a standard go-to method to assess the radiocarpal joint.
Our Technique
- Begin by scanning the unaffected wrist to visualize normal anatomy. The hand should be pronated. Support the wrist on a flat surface in slight flexion using a towel roll. Using a high-frequency (15–6 MHz) linear transducer in the transverse plane, begin in the distal one-third of the forearm and scan distally to identify the second compartment of the extensor tendons of the wrist. Use Lister’s tubercle as the landmark for the most ulnar aspect of the second compartment, which is composed of the extensor carpi radialis brevis and extensor carpi radialis longus tendons (see Figure 1B). Rotate the transducer to the longitudinal orientation (ie, with the probe marker facing the fingertips), and slide the transducer in a distal manner over the radius and carpus in line with the middle finger, allowing you to visualize the distal radius and the scaphoid. Scan toward the thumb to visualize the entire distal radius. There should be minimal hypoechoic (dark) signal in the radiocarpal space. Also note the overlying extensor tendons (see Figure 2).
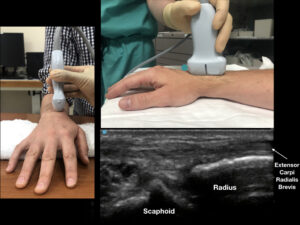
- Now scan the affected wrist using the same technique. An effusion will appear as a hypoechoic (dark) space between the distal radius and the carpal bones (see Figure 3).
- For aspiration, the following supplies are required (we recommend using standard sterile procedure for all joint aspirations): a disinfection solution (such as chlorhexidine), sterile gel, a sterile probe cover, 5 cc of local anesthetic with a 25-g syringe (for an anesthetic skin wheal), and a 5–10-cc syringe with an 18-g needle for aspiration.
- Prep the patient for aspiration. Clean a generous area on the dorsal wrist with chlorhexidine and allow it to dry. Place a sterile sheath over the linear probe and use sterile gel to visualize the effusion again.
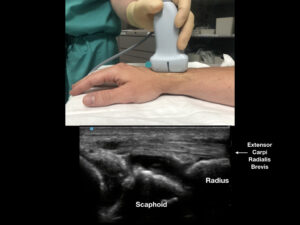
- Using your nondominant hand, scan over the effusion in the longitudinal plane to achieve excellent visualization of the extensor carpi radialis brevis tendon. Maintain the probe in this position. Done correctly, the probe serves to guard the underlying tendon during aspiration, decreasing the likelihood of tendon puncture with aspiration needle.
- Use M mode or center line on the ultrasound system to show the probe’s midline on the ultrasound display. Using a 25-g needle, place a small subcutaneous skin wheal at the injection site (radially adjacent to the ultrasound probe). Then using an 18-g needle on a 5–10-cc syringe, enter the skin at a steep (70–90º) angle, using an out-of-plane approach. You may visualize the needle tip as it enters the effusion. Gently aspirate as you enter and obtain as much fluid as possible (see Figure 4).
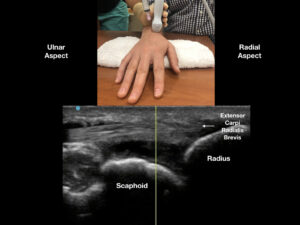
Figure 4: With the ultrasound probe covering the extensor carpi radials brevis, enter the swollen joint capsule with an out-of-plane technique. We recommend a steep needle angle of entry between Lister’s tubercle and the extensor carpi radials brevis. The procedure should be performed with sterile precautions (like any other joint aspiration). Credit: Arun Nagdev
Conclusion
The simplified technique described here gives clinicians inexperienced with wrist aspirations a reliable method to easily detect the presence of a joint effusion and, as needed, to enter the joint capsule with reduced risk of injury to tendons and vasculature. In our experience, this technique has been invaluable in the evaluation of patients with a painful and swollen distal forearm or wrist in our emergency department. In most cases, the clinician uses their physical exam in conjunction with ultrasound of the radiocarpal joint to determine the need for aspiration. In cases with a clear radiocarpal joint effusion, our novel, easy technique ensures successful joint fluid aspiration.
Bottom line: Ultrasonographic evaluation of a painful wrist and ultrasound-guided aspiration of a wrist effusion are well within the emergency physician skill set. Add it to your armamentarium.
References
- Balint PV, Kane D, Hunter J, et al. Ultrasound guided versus conventional joint and soft tissue fluid aspiration in rheumatology practice: a pilot study. J Rheumatol. 2002;29(10):2209-2213.
- Berona K, Abdi A, Menchine M, et al. Success of ultrasound-guided versus landmark-guided arthrocentesis of hip, ankle, and wrist in a cadaver model. Am J Emerg Med. 2017;35(2):240-244.
Dr. Henry is a senior resident in the emergency department at Highland General Hospital in the Alameda Health System in Oakland, California.
Dr. Nagdev is director of emergency ultrasound at Highland General Hospital in the Alameda Health System in Oakland, California.
Pages: 1 2 3 | Multi-Page




No Responses to “Easy Ultrasound Technique to Evaluate and Aspirate an Atraumatic Painful Wrist”