Patients who have been discharged from the emergency department and rapidly return for another complaint present a challenge to the emergency physician. It is frustrating to see a patient return so quickly after spending hours on a thoughtful and thorough workup. However, it is important to consider the circumstances of their return and focus on any change in their condition that might necessitate a new approach. This case illustrates the medicolegal risk involved in rapid patient bouncebacks, handoffs, and safe discharge planning.
Explore This Issue
ACEP Now: Vol 39 – No 06 – June 2020The Case
A 70-year-old male presented to an emergency department by private vehicle with a chief complaint of left leg pain. He had a history of atrial fibrillation for which he was prescribed warfarin. Approximately one week before the ED visit, he had been walking on a deck and fell about two feet to the ground. He had ongoing left leg pain from his knee to his ankle. On arrival to the emergency department, he was using crutches and was helped into a wheelchair by ED staff.
The patient was seen by a physician. His initial vital signs were unremarkable, and his pain was rated as 9/10 in the left leg. He was noted to have left leg bruising and severe unilateral edema. A neurovascular exam was normal. The remainder of the physical exam was normal. Multiple tests were ordered, including a complete blood count (CBC), comprehensive metabolic panel (CMP), coagulation panel (the patient was anticoagulated on warfarin for atrial fibrillation), ultrasound for deep venous thrombosis (DVT), chest X-ray, and left tibia/fibula X-ray.
Figure 1 shows the X-ray results. The results were significant for an international normalized ratio (INR) of 1.5. The CBC and CMP were unremarkable. The lower extremity imaging did not show any fractures.
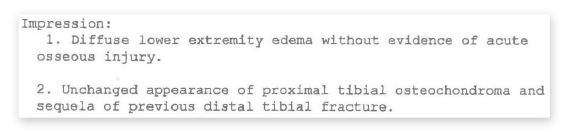
Figure 1: The patient’s X-ray results.
Unfortunately, obtaining the DVT exam was complicated. The facility at which the patient was seen did not have an ultrasound technician, so to get an ultrasound performed and read by a radiologist, the patient was transferred to another hospital to undergo the ultrasound study, then returned to the original emergency department to wait for results.
Prior to the patient leaving to get the DVT ultrasound, the physician ordered 5 mg of oral warfarin and 100 mg of subcutaneous enoxaparin (Lovenox) to treat the patient’s subtherapeutic INR (see Figure 2). Additionally, 80 mg of furosemide (Lasix) was ordered to treat his edema. While the patient was away at the other facility getting the DVT ultrasound, there was a shift change and the original physician signed out the patient’s care to the oncoming doctor.
Pages: 1 2 3 | Single Page





One Response to “Elderly Patient Dies after Emergency Dept. Bounceback, Lawsuit Results”
July 13, 2020
Dan Magdziarz, DOGreat insights with this article Dr. Funk – take home points we should all keep in mind => 1) Obtaining CT head is key with head-injury patients on anticoagulation (especially the elderly) – no matter how “good” they may look. 2) Placing a knee immobilizer on an elderly patient is one of those few instances in Emergency Medicine where “over-doing” can actually get you (and your patients) in trouble. 3) Charting a disposition re-exam may go a long way in decreasing your medical-legal risk (ie. “The patient was observed ambulatory using crutches with steady gait” >> “crutches ordered”). Thanks for keeping us focused to practice our best!