Patients who have been discharged from the emergency department and rapidly return for another complaint present a challenge to the emergency physician. It is frustrating to see a patient return so quickly after spending hours on a thoughtful and thorough workup. However, it is important to consider the circumstances of their return and focus on any change in their condition that might necessitate a new approach. This case illustrates the medicolegal risk involved in rapid patient bouncebacks, handoffs, and safe discharge planning.
Explore This Issue
ACEP Now: Vol 39 – No 06 – June 2020The Case
A 70-year-old male presented to an emergency department by private vehicle with a chief complaint of left leg pain. He had a history of atrial fibrillation for which he was prescribed warfarin. Approximately one week before the ED visit, he had been walking on a deck and fell about two feet to the ground. He had ongoing left leg pain from his knee to his ankle. On arrival to the emergency department, he was using crutches and was helped into a wheelchair by ED staff.
The patient was seen by a physician. His initial vital signs were unremarkable, and his pain was rated as 9/10 in the left leg. He was noted to have left leg bruising and severe unilateral edema. A neurovascular exam was normal. The remainder of the physical exam was normal. Multiple tests were ordered, including a complete blood count (CBC), comprehensive metabolic panel (CMP), coagulation panel (the patient was anticoagulated on warfarin for atrial fibrillation), ultrasound for deep venous thrombosis (DVT), chest X-ray, and left tibia/fibula X-ray.
Figure 1 shows the X-ray results. The results were significant for an international normalized ratio (INR) of 1.5. The CBC and CMP were unremarkable. The lower extremity imaging did not show any fractures.
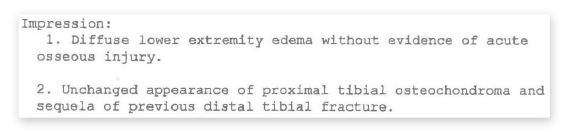
Figure 1: The patient’s X-ray results.
Unfortunately, obtaining the DVT exam was complicated. The facility at which the patient was seen did not have an ultrasound technician, so to get an ultrasound performed and read by a radiologist, the patient was transferred to another hospital to undergo the ultrasound study, then returned to the original emergency department to wait for results.
Prior to the patient leaving to get the DVT ultrasound, the physician ordered 5 mg of oral warfarin and 100 mg of subcutaneous enoxaparin (Lovenox) to treat the patient’s subtherapeutic INR (see Figure 2). Additionally, 80 mg of furosemide (Lasix) was ordered to treat his edema. While the patient was away at the other facility getting the DVT ultrasound, there was a shift change and the original physician signed out the patient’s care to the oncoming doctor.

Figure 2: The physician’s warfarin and Lovenox order.
After the patient’s return, the ultrasound results were finalized and were negative for DVT. The patient was placed in a knee immobilizer and discharged to follow up with orthopedics. He was offered a wheelchair but declined in favor of using his crutches. While he was making his way out of the front of the hospital, the patient lost his balance, fell, and hit his head on the ground. A nurse witnessed this, and he was brought back into the emergency department and evaluated by the same physician who had discharged him only minutes earlier.
The patient denied loss of consciousness, and his vitals were again unremarkable. An abrasion to the head was noted, but otherwise he had a normal exam and no complaints. He was discharged home without any further workup.
The patient made it back to his apartment. The next morning, a friend was unable to contact him and went to check on his well-being. Unfortunately, he was found dead. An autopsy was performed, and a large subdural hematoma was discovered (see Figure 3).

Figure 3: The patient’s autopsy report.
Legal Blowback
The patient’s family filed lawsuits against the nurses involved as well as the physician who discharged him. The lawsuit was filed in federal court because the emergency department was a Veterans Affairs facility. Ultimately, the federal case was dismissed without trial. The case against the physician was then refiled in state court, and an undisclosed settlement was reached prior to trial.
This case illustrates several key points. Although some emergency physicians comfortably perform DVT exams at the bedside, many are not in the practice of doing so or were trained before point-of-care ultrasound was in wide use. Performing a DVT study at the bedside could have been completed in just a few minutes, negating the need to transfer this patient. The argument can be made that he would not have required empiric anticoagulation while waiting for transfer and there would also not have been a handoff of his care.
The patient presented back to the emergency department only several minutes after having been discharged. Every ED physician knows the frustration of a rapid bounceback. After a patient has a long ED stay with a complicated workup, it can be difficult to start over again with an entirely new workup for a new chief complaint. However, it is important to avoid early mental closure in these situations and not brush off a subtle but life-threatening presentation. Working quickly toward a rapid disposition is an important skill in emergency medicine, but it must be balanced against the risks of causing harm.
In hindsight, it is obvious the patient needed a CT scan of his head. He was an elderly patient on warfarin, and due to his subtherapeutic INR, he had been given additional anticoagulation hours before his head injury. There are no clinical decision rules that would suggest this patient could safely be discharged without obtaining a head CT.
Another possible contributing factor to his fall was the fact he was placed in a knee immobilizer. An elderly man on anticoagulation with limited mobility is an obvious fall risk. There is no indication for using a knee immobilizer in this case given that he did not have any fractures or injury to the extensor mechanism of his knee. Simple compression with an ACE bandage would have been appropriate and allowed for safer mobility.
See the Records
To read more details on the lawsuit, click here.
 Dr. Funk is a practicing emergency medicine physician in Springfield, Missouri, and owner of Med Mal Reviewer, LLC. He writes about medical malpractice at www.medmalreviewer.com.
Dr. Funk is a practicing emergency medicine physician in Springfield, Missouri, and owner of Med Mal Reviewer, LLC. He writes about medical malpractice at www.medmalreviewer.com.
Pages: 1 2 3 | Multi-Page




One Response to “Elderly Patient Dies after Emergency Dept. Bounceback, Lawsuit Results”
July 13, 2020
Dan Magdziarz, DOGreat insights with this article Dr. Funk – take home points we should all keep in mind => 1) Obtaining CT head is key with head-injury patients on anticoagulation (especially the elderly) – no matter how “good” they may look. 2) Placing a knee immobilizer on an elderly patient is one of those few instances in Emergency Medicine where “over-doing” can actually get you (and your patients) in trouble. 3) Charting a disposition re-exam may go a long way in decreasing your medical-legal risk (ie. “The patient was observed ambulatory using crutches with steady gait” >> “crutches ordered”). Thanks for keeping us focused to practice our best!