Emergency departments face significant challenges in patient management and concomitant increases in regulatory and reporting requirements. Some regulatory requirements are matched to transparency mandates for items that will be reported to the public, such as the Hospital Compare measures from the Centers for Medicare and Medicaid Services. And notably, the issues of timely care, flow through the emergency department, and safety incidents in the ED waiting room have activated regulators, The Joint Commission, and the general media.
Explore This Issue
ACEP Now: Vol 37 – No 11 – November 2018ED leaders have tackled the critical imperative to reduce the number of persons who enter the emergency department but leave prematurely. The Emergency Department Benchmarking Alliance (EDBA) has worked with other organizations to develop definitions that provide consistency in reporting. With the input of ED leaders who recognize the temptation to cheat on this reporting element, it was necessary to develop an inclusive term that would incorporate all patients who leave before they are supposed to and would not provide gaps for patient encounters to be missed in the ED reporting systems.
The participants in the third Performance Measures and Benchmarking Summit have published the results of the sessions in which ED definitions were developed, with incomplete ED patient encounters termed “left before treatment complete” (LBTC).1 This single definition provides the most complete accounting for all patients who leave the emergency department before they are supposed to, and it includes patients who leave before or after the EMTALA-mandated medical screening examination, those who leave against medical advice (AMA), and those who elope (ie, simply walk out without speaking to anyone).
The EDBA uses this single statistic to compile the annual number of patients who are recognized by the emergency department but leave prior to completion of treatment. This provides the most complete accounting for all incomplete encounters, and it delivers a great comparison statistic.
The Stats
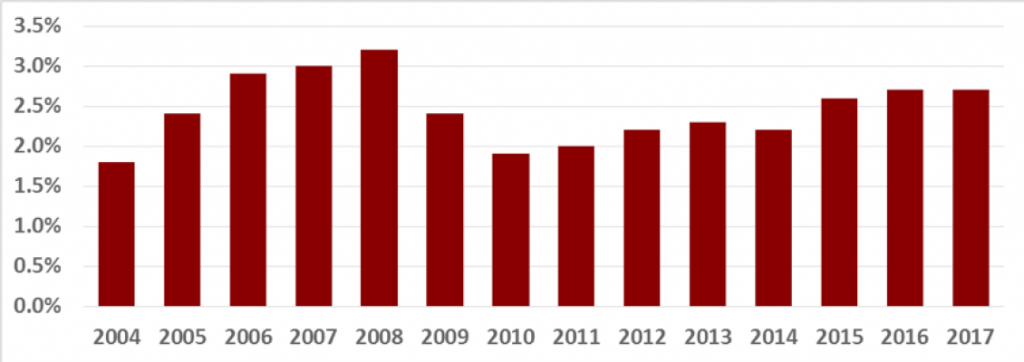
A number of studies have related ED walkaway rates to flow rates, and across a 14-year time frame, the EDBA data have found walkaway rates relate to volume, ED type, time to first contact with a licensed provider, and overall ED flow.2,3 The LBTC rate has trended lower across EDBA hospitals over the prior 14 years (see Figure 1).
For the past eight years, the EDBA study has evaluated various time intervals and their potential contribution to the LBTC rate. Table 1 shows the eight-year data on LBTC and median door-to-provider and door-to-decision times for admitted patients. Despite a consistent drop in median door-to-provider times, the LBTC rate has gone up, possibly because during those eight years the door-to-decision time has crept higher. That time is generally under the control of the emergency physician, and it offers an opportunity to focus on efficiencies that will move critical information to emergency physicians so they can make a quality decision.
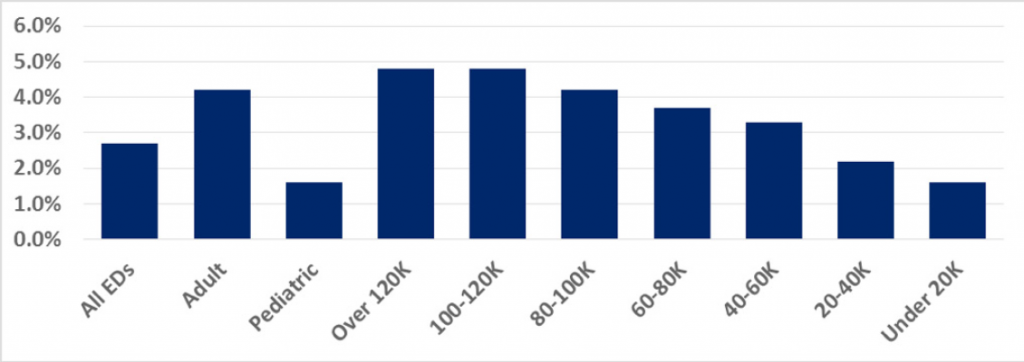
In 2017, the LBTC rate was 2.7 percent across all emergency departments, but it varied significantly across the various cohorts that represent different types of emergency departments and different ED volumes. The LBTC rate by cohort appears in Figure 2.
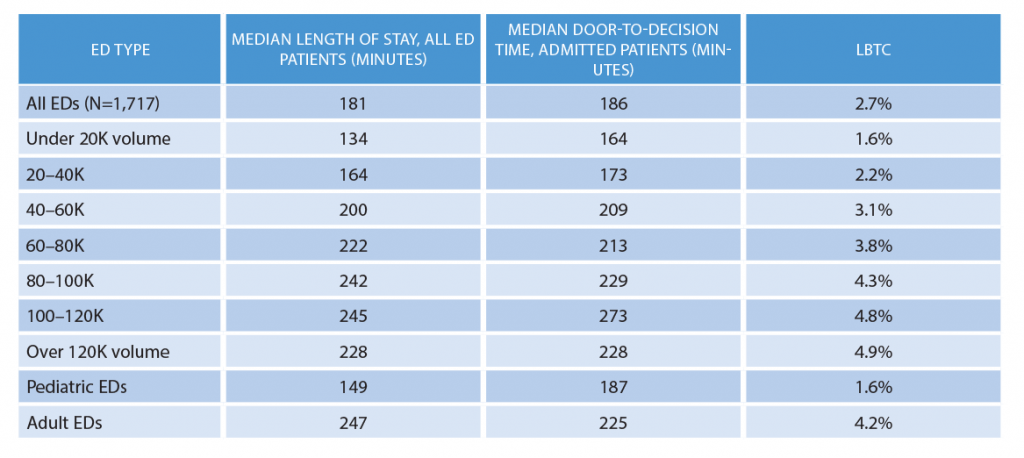
(click for larger image) Table 2: 2017 Emergency Department Benchmarking Alliance Data Survey Results
Table 2 shows the EDBA time intervals and LBTC rate. That data suggests a correlation between processing all patients, the door-to-decision time for admitted patients, and overall walkaway rates. And it clearly reflects the stresses on ED operations when volume and patient acuity increase.
The overall complexity of processing patients who ultimately are admitted is reflected in the amount of time it takes across all cohorts to arrive at the decision to admit. Even in the smallest emergency departments, the median time to that decision was 164 minutes. The other ED cohorts reported a time range of roughly 180–228 minutes, except for the group of emergency departments in the 100,000–120,000 volume range, where the time to decision averages 273 minutes. Long time intervals to decision to admit or discharge are associated with higher LBTC rates.
Conclusions
We can see emergency physicians have an opportunity to reduce walkaway rates by improving decision timing. Many emergency departments have reduced door-to-provider time, but we also need a timely effort to perform diagnostic testing and get the results to the responsible emergency physician, initiate any necessary treatment and evaluate the results, conduct necessary conversations with primary care or other consulting physicians, and complete a review of pertinent medical records. All of those items combined will give the emergency physician an opportunity to make a quality disposition decision and initiate transition of care.
Decision to admit by an emergency physician begins a cascade of events that should end in a timely movement of the patient to the inpatient unit. A boarding time discussion took place in a 2016 ACEP Now article, but unfortunately the EDBA boarding time numbers in 2016 and 2017 remained consistent at about 117 minutes.4
Despite ED volume and acuity increases that challenge ED providers, improved operations have been evident in many emergency departments. However, the LBTC rates relate to ED efficiency and processing, and improving those areas requires coordinated utilization of staff, equipment, processes, and documentation.
Bottom line: Opportunities to improve patient flow do exist, and improved patient flow will reduce the rate of incomplete patient encounters.
References
- Wiler JL, Welch S, Pines J, et al. Emergency department performance measures updates: proceedings of the 2014 Emergency Department Benchmarking Alliance consensus summit. Acad Emerg Med. 2015;22(5):542-553.
- Sun BC, Binstadt ES, Pelletier A, et al. Characteristics and temporal trends of “left before being seen” visits in U.S. emergency departments, 1995–2002. J Emerg Med. 2007;32(2):211-215.
- Anderson D, Pimentel L, Golden B, et al. Drivers of emergency department efficiency: a statistical and cluster analysis of volume, staffing, and operations. Am J Emerg Med. 2016;34(2):155-161.
- Augustine JJ. Long ED boarding times drive walkaways, revenue losses. ACEP Now. 2016;35(7):16.
Pages: 1 2 3 | Multi-Page






One Response to “Emergency Department Inefficiency Drives Poor Quality”
December 2, 2018
Rob Beatty, MD FACEPGood article. In the time frame reported, there has been a major push for EMR conversion due to meaningful use requirements. Some of those EMRs impact house-wide processes as a whole, which could cause significant increases in lab/radiology turnaround time, and add additional human steps to workflow that were not in practice previously. Have you considered evaluating these additional data points and seeing how they fit into your analysis?