Explore This Issue
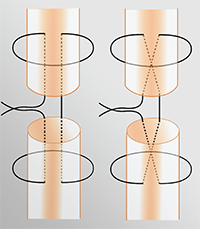
ACEP Now: Vol 34 – No 12 – December 2015Figure 3. The modified Kessler (left) and modified Bunnell (right) stitches for tendon repair.11
Image Credit: Justin McNamee
Zone IV: Once you start to enter zone IV, the tendons become larger and easier to repair. Fortunately, there are not many instances of closed tendon injuries from zone IV and the more proximal zones. For tendon lacerations that are greater than 50 percent of the tendon, we can repair the tendon with the modified Kessler technique detailed below in the suturing technique section.8 Similar to zone III injuries, these should also be splinted in a volar splint and should follow up with the hand surgeon on an outpatient basis.10
Zone V: This zone is where we frequently encounter the “fight bites” that patients don’t always willingly admit. With the high possibility of subsequent complications, any open injury in this region should be treated as a fight bite until proven otherwise. After extensive irrigation of the wound, we can suture the tendon if possible. However, leave the skin open for hand surgeons to do a delayed closure in their office. This is in addition to placing a splint (wrist in 45° of extension, MCP in 20° of flexion) and starting patients on prophylactic antibiotics, such as Augmentin.5 If patients aren’t going to see the hand surgeon the next day, it may be prudent to have them come back to the ED for a wound check in the next 24 hours.
Using the modified Bunnell technique and 4-0 nonabsorbable sutures, we can repair these lacerations in the ED. Patients can then be splinted (wrist in 30° of extension, MCP neutral, DIP and PIP joints free) and follow up with a hand surgeon.
Zone VI: This zone encompasses the majority of the dorsum of the hand. The broad, well-defined tendons in this area make it, arguably, the easiest tendon repair we can do in the ED. Using the modified Bunnell technique and 4-0 nonabsorbable sutures, we can repair these lacerations in the ED. Patients can then be splinted (wrist in 30° of extension, MCP neutral, DIP and PIP joints free) and follow up with a hand surgeon.10
Zones VII and VIII: Once you have an extensor laceration in the wrist or forearm, the musculotendinous junctions and muscle bellies become more involved, which is outside of the scope of what we can repair in the ED. We should repair the overlying skin and put in a volar splint (wrist in 20° of extension, MCP neutral). Our hand surgeon colleagues are going to need to repair these injuries.10
Tendon-Suturing Techniques
As described above, there are a number of different ways to repair tendon lacerations. Typically, the tendon should be repaired with 4-0 or 5-0 nonabsorbable sutures. Two of the more commonly described repairs are the modified Kessler and modified Bunnell stitches. Figure 3 provides a schematic of the repair.
Modified Kessler Stitch
Modified Bunnell Stitch
Summary
Far too often, we become reliant on our consultants for relatively simple procedures that can be done safely and efficiently in the ED. Figure 4 provides a quick reference for repairing these extensor tendon injuries in the ED; it is assumed that all of these injuries are adequately irrigated and debrided and that the patient’s tetanus status is updated. For the majority of these injuries, you can approximate the overlying skin laceration, splint, and have the patient follow up with the hand surgeon in the next couple of days. These injuries can be repaired as late as one week after the initial injury.9 Instead of waking up the orthopod at 3 a.m. for someone’s drunken stupor–fueled flight through a pane of glass, just take matters into your own hands.
Pages: 1 2 3 4 | Single Page





No Responses to “Emergency Department Management of Extensor Tendon Lacerations”