Explore This Issue
ACEP Now: Vol 34 – No 11 – November 2015(click for larger image)
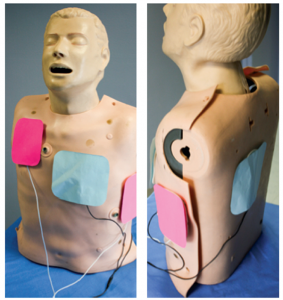
Figure 1. Orientation of defibrillation pads for double sequential external defibrillation: anterior-posterior (blue) and anterior-apex (pink).
phenomenon in the medical literature. It has been studied and theorized for well over a decade. Most of the current literature agrees on one concept: an ES activates the sympathetic nervous system and, in turn, leads to a surge of endogenous catecholamines.2 The abundance of endogenous catecholamines is likely the underlying culprit as to why conventional ACLS doesn’t lead to ROSC in the majority of these patients. The ACLS algorithm for VF/ventricular tachycardia (VT) calls for 1 mg epinephrine to be given every three to five minutes; there isn’t an asterisk next to this recommendation for patients in refractory VF arrest stating we should consider holding this medication or trying a different medication in our armamentarium. The addition of exogenous catecholamines in patients in refractory VF arrest or ES seems counterintuitive to what we know about this phenomenon. In fact, a better solution may be to give the patients a class of medications that suppresses the adrenergic surge they are experiencing, namely β-blockers.
The Hail Mary: Esmolol and Double Sequential External Defibrillation
A 2014 study in the journal Resuscitation retrospectively looked at patients in refractory VF arrest and compared those who received standard ACLS therapy against standard therapy followed by esmolol.3 Driver et al defined refractory VF arrest as patients with an initial presenting rhythm of VF or VT who received at least three defibrillation attempts, 3 mg adrenaline, and 300 mg amiodarone and remained in VF cardiac arrest upon arrival in the ED. In this Resuscitation study, a bolus of 500 mcg/kg (0.5 mg/kg) esmolol was administered followed by a continuous infusion of esmolol from 0–100 mcg/kg/min (0–0.1 mg/kg/min) to the study group, while the control group only received medications via the ACLS protocol. Of those in refractory VF arrest who received esmolol, 67 percent had ROSC compared to 32 percent in the standard therapy arm, and 50 percent of the esmolol group survived to discharge with good neurological outcome (CPC score <2) compared to 11 percent in the standard therapy group. While this was a small retrospective study on refractory VF arrest in the ED, the results were in alignment with previous case reports dating back to the 1960s. Furthermore, studies not centered in the ED have used β-blockers for refractory ES, such as the Nademanee et al study in Circulation in 2000 and Miwa et al in 2010.1,3,4 The study results provide a measurable benefit in favor of using β-blockers to counteract the endogenous and exogenous (if given) catecholamine surge theorized to occur during refractory VF arrest. Even though the current evidence for the use of esmolol in refractory VF arrest is far from concrete, it still far exceeds the evidence we have for other chemical agents to use on patients who do not respond to the traditional ACLS antidysrhythmics. However, the use of β-blockers may not be the only option and could possibly be used in combination with another piece of equipment readily available in the ED when the next refractory VF arrest presents to your ED.
With very little downside of employing these interventions in refractory VF arrest patients, ED providers can try this Hail Mary to treat the patient’s electrical storm.
(click for larger image)
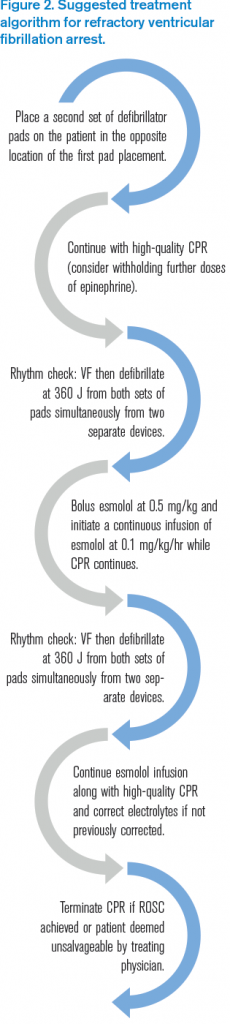
Figure 2. Suggested treatment algorithm for refractory ventricular fibrillation arrest.
Pages: 1 2 3 4 | Single Page





3 Responses to “Emergency Interventions for Treating Cardiac Electrical Storms”
January 13, 2016
Steven SawyerI read this article this past weekend and knew that even though I had never seen a case of refractory Vfib I knew I would shortly. So I was not actually surprised when the 45 year old man brought in cardiac arrest had Vfib for which he had received two doses of epi and three shocks by ems. An LMA was in place and while cpr continued I had to wait to see the monitor. During a change in compression hands I saw the fine vfib and delivered another defib with epi and amiodarone to no avail. During the next cycle I had a chance to brief the team on the article I had read and get a copy so we could check the dose of Esmolol while maxing the amiodarone and applying the 5th shock. However, it turned out that we had no Esmolol in the ED. At this point it was 30 since being found down. I set the two defibrillators and performed the double sequential external defibrillation which initially converted from fine vfib to asystole After additional CPR and an additional attempt the code was called. It turned out that the pt had initially been over come with carbon monoxide which lead directly to his cardiac dysrhythmia. Had I known this I may have elected to remove the LMA and intubate for better oxygen support. But overall my team was fast and compliant with the strange instructions I gave. It just didn’t work this time.
March 7, 2017
günther krumpl0–100 mcg/kg/hr (0–0.1 mg/kg/hr)
Please correct the text in the publication to the right dose which should be
0-100 mcg/kg/min.
In addition I want to mention that 0 in 0-100 makes no sense, the starting dose of esmolol is 50. So it should say 50-100 …
April 14, 2017
Dawn Antoline-WangThank you, the article has been updated to indicate mcg/kg/min instead of mcg/kg/hr.