Emergency medicine (EM) has evolved over time and has long passed a crossroads where previously unachievable capabilities should be celebrated and shared. Emergency physicians have become leaders in achieving cost efficiency in health care, predominantly through implementation of new processes and research findings, enabling us to achieve significant financial savings.
Explore This Issue
ACEP Now: Vol 42 – No 07 – July 2023Emergency physicians have earned the right to “re-brand” ourselves as indispensable, money-saving change agents in the health care enterprise.
Of course, the bill for any episode of emergency department (ED) care can be substantial, exceeding the billed charges for equivalent care provided in some primary care offices. Thus, the idea that we are leaders at achieving cost savings may at first seem counterintuitive.
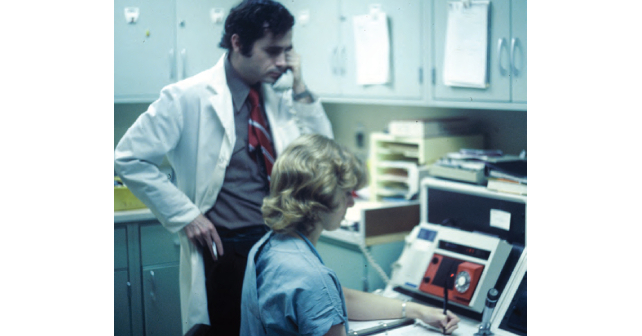
However, such a view overlooks two critical facts. First, much of the care we provide could not be provided in an office. Second, as cited above, we have implemented research findings to decrease costs of care safely, via processes that did not exist at the time the American Board of Emergency Medicine became recognized by the American Board of Medical Specialties in 1979, or even at the time I entered emergency-medicine residency training in 1986.
After convincing ourselves that we save our systems large sums of money, we need to educate our critics. We don’t deserve the recurrent blame and scorn from individuals who shape public opinion, including some politicians and journalists, who repeatedly focus on the charges accrued for ED care, with only passing acknowledgement of the critical role we all play as the nation’s 24/7/365 resource for medical care for all who present at our doors, without regard for their ability to pay.
Here are some illustrative examples demonstrating how emergency physicians save our system money every day, compared to status quo of the late 1970s and early 1980s: Formerly, nearly all acute pyelonephritis patients were admitted for several days of intravenous (IV) antibiotic therapy. Now, many acute pyelonephritis patients receive an IV antibiotic, analgesia, and an antiemetic in the ED. Once patients demonstrate they can keep oral liquids down, most are prescribed oral antibiotics, analgesics and antiemetics, and discharged. Acute pyelonephritis has become a disease for which outpatient management is often feasible and appropriate.1
Formerly, most patients with Pelvic Inflammatory Disease (PID) were admitted for several days of IV antibiotics, under the now-disproven dogma that IV antibiotics decreased the scarring of the Fallopian tubes and enhanced the patient’s future fertility. Now, many PID patients are treated and released after ED administration of appropriate antibiotics to eradicate possible infection by Neisseria gonorrhea and Chlamydia trachomatis, often with added treatment for anaerobic microbes. Female upper genital tract disease has been transformed to a disease for which outpatient management is often feasible and appropriate.2
Pages: 1 2 3 4 | Single Page




No Responses to “Emergency Medicine Deserves to “Re-Brand” Itself as a Cost Saver”