For many emergency physician parents, the COVID-19 crisis has placed them in the unique position of managing not only the stress of caring for patients on the front lines, but also caring for their families at home. It prompted new concerns about their own safety and that of their families. Schools shut down, normal routines were thrown out the window, face masks became de rigueur. EM families experienced the disruption, but with an added layer of concern for their loved ones on the front lines.
Explore This Issue
ACEP Now: Vol 39 – No 05 – May 2020ACEP Now spoke with several emergency physicians to hear what has helped them explain this pandemic—and their important role in fighting the virus—to their children of all ages.
Contributors
- Vonzella Bryant, MD, FACEP, EM clerkship director at Boston Medical Center/Boston University School of Medicine, with two children (ages 12 and 10)
- Ari Gotlib, MD, EM faculty at McLaren Oakland Hospital in Pontiac, Michigan, with four children (ages 10, 8, 8, 4)
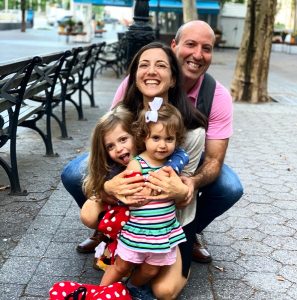
- Jordana Haber Hazan, MD, FACEP, and Alberto Hazan, MD, emergency physicians in Las Vegas with two daughters (ages 4 and 2)
- Howie Mell, MD, MPH, CPE, FACEP, an emergency physician who works in St. Louis but lives in North Carolina, with four children (ages 14, 12, 10, 7)
- Christina Shenvi, MD, PhD, FACEP, professor, associate residency director for the University of North Carolina Department of Emergency Medicine, with four children (ages 11, 9, 7, 5)
- Michael Wilson, MD, locums physician from Tyler, Texas, with seven children (ages 18, 16, 14, 7, 5, 18 months, 6 months)
COVID Conversations: Every Kid is Different
Maybe future parenting books will include a chapter titled “How to Solve the Pandemic Parenting Puzzle,” but for now, physician parents are left without a standard pathway. Still, they agreed that communication has to be tailored to each child depending on age, personality and family circumstances.
When Dr. Wilson volunteered for a three-week assignment in New York City to care for COVID-19 patients, he and his wife discussed the disease with their older kids differently than with the younger children. “I told them, ‘It’s a really bad disease that is killing a lot of people. At the same time, we know that if we are given talents and tools to help, we can’t sit here and watch other people suffer.’” Dr. Wilson said they talked about it in context of their religious beliefs, discussing how important it is to “step up and do something” if you can lessen someone’s pain and suffering.
Dr. Mell said his older children ask a lot of scientific questions such as, “Why can’t we use radiation?” and “Did you intubate any patients last night?” while his younger children are more concerned with whether they’re allowed to hug him when he gets home from work.
In Dr. Shenvi’s household, her husband is in the middle of treatment for a brain tumor, so their children are already accustomed to having honest conversations about mortality. That groundwork probably made the COVID-19 discussions easier, Dr. Shenvi said. “I think it’s less important what we say and more important how we are acting, because [our children] will take their cues from us,” she said. She and her husband are staying calm and trying to maintain normalcy. “We’re not, you know, hoarding toilet paper,” she joked.
Dr. Gotlib and his wife, a home care nurse who is also working a lot during this crisis, are seeing their kids’ personalities react very differently to the stress of a global pandemic. His 8-year-old daughter is completely unfazed, while her twin brother is a different story.
“He asks me every day what my shift is. He wants to know when I’m leaving, and when I’m coming back. He wants to know if I’m on an 8, 10, or 12,” Dr. Gotlib said. “It worries me how he’s taking it, because he seems to be getting more introverted and anxious as this [crisis] progresses. We do our best, but when we’re solo [parenting] whenever we’re home, it makes it hard to focus. We try to reassure him the most that everything is fine, that mom and dad are safe, that we’ll always be there for him. We try and avoid having work conversations when he’s around.”
The Gotlibs also have a 10-year old son who is deeply curious about his parents’ role as health care workers during this pandemic. “He’s a really emotional kid, and he gives me big hugs every night,” Dr. Gotlib said. “I don’t think he realizes those hugs support me as much as they support him.”
When in Doubt, Demonstrate
For many kids, seeing is believing. When it comes to quelling COVID-19 fears, many emergency physician parents deployed a similar teaching tactic: They brought out the personal protective equipment (PPE). They donned and doffed, showed their kids the various masks and goggles, explained how each piece worked, and walked the children through the post-shift decontamination process.
“I put [my PPE] on for them, and I was actually wearing it around the house,” said Dr. Mell, noting that his kids agreed the gear makes him look like Bane from the Batman movies. When he and his wife, Deb, learned of the PPE shortage in some hospitals, their kids helped them ship extra masks to emergency physicians in need. Ms. Mell said she thought it made their children feel better because they were doing something to contribute, just like their father.
When he heard his 7-year old praying that the coronavirus wouldn’t kill anyone in their family, Dr. Wilson wanted to do something to lessen her fears. He spread 100 pieces of cereal on the table in front of his younger children, each one representing a person with COVID-19. He separated the pieces into piles to show how many are asymptomatic, mildly ill, dying, already have chronic illness, are over a certain age, etc. Seeing the visual demonstration “helped them process [our risk],” Dr. Wilson said.
For the physicians with younger children, the key messages are simple and interactive. The Hazan daughters are just 4 and 2 years old, so it’s all about teaching them about health and hygiene in a fun, lighthearted way. “We ask them about what we do to stay healthy and prevent germs from spreading. We talk about properly washing our hands, and this has been fun for them,” said Dr. Haber Hazan. “My daughter has shown me how to wash my hands between each finger and on both sides; she loves to correct me when I’m not doing this properly.”
It can be hard for young children to remember not to run straight into their parents’ arms when they get home. “We’ve told them to be the ones to remind us to shower right away when we get home. This puts them in charge,” Dr. Haber Hazan said. “When I enter the house, I get immediate orders to go right upstairs to wash the germs from the hospital.”
A New Normal at Home
Dr. Bryant’s family shares a home with her mother, who had COVID-like symptoms after returning from a trip abroad. Because she worried her mother may have had the virus, Dr. Bryant carefully explained to her kids why they would be quarantining very strictly to prevent spreading it to others. She said her children have taken it in stride for the most part, although there has been an uptick in sibling arguments.
For her, the hardest part is suddenly homeschooling her stir-crazy children while balancing her work responsibilities. Her advice to other emergency physicians trying to balance it all? “Pace yourself, just like we do with busy shifts in the ED. It’s going to be a marathon and not a sprint,” she said. “If we are anxious, our kids are going to be anxious. Like the motto in our ED, we have to ‘Keep Calm and Trauma On.’ Which, in this case, the trauma is managing family life in the time of COVID.”
Dr. Shenvi said she is staying focused on the facts and what is within her circle of control. “There’s lots of things that I’m concerned about—the economy or unemployment or people who have serious illnesses—that I can’t affect at all. The only things I can control are what I do with my family, my house, my time, my energy. And so, I’m going to focus on making that as supportive to my family as possible.”
Working with Unfamiliar Worries
Many emergency physicians are used to accepting some risk when they go to work, but it’s a very different feeling to worry about bringing the virus home to their families.
“We’re used to doing dangerous things ourselves. Oftentimes, the enemy is over and done with the by the time we’re even seeing the patient. The hurricane’s done, the earthquake, the fire, the shooting,” Dr. Wilson said. “When the patient comes with the enemy still [present], you know, that’s a hard war to fight.”
Dr. Gotlib acknowledged the new burdens he’s feeling: “Knowing that, while I’m telling my kids I’ll always be there for them, I still more than doubled my life insurance and disability a month ago. Knowing that I’m intubating COVID patients daily with PPE that I purchased myself and then coming home to them hoping no one gets sick or they don’t carry it to someone else.” Still, he said he’s thankful to have a job when many in the country don’t, and spending this extra time with his family reminds him how fortunate he is to have a great support system.
Dr. Haber Hazan said she and her husband, who is also an emergency physician, are definitely experiencing fear and uncertainty, but their kids have inspired them with their resiliency and willingness to accept change. “We are grateful for time together at home where we can slow down and reflect on what is most important to us,” she said. “While we worry about protecting them from COVID-19—both emotionally and physically—our children have served as a reminder to find joy in this moment.”
Ms. Grantham is ACEP’s communications manager.










No Responses to “Emergency Physician Parents Share How They’re Managing the COVID-19 Crisis”