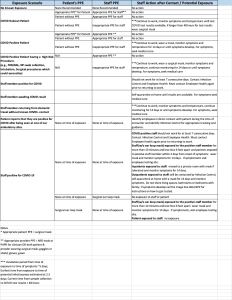
Appropriate personal protective equipment (PPE) is required to safely care for patients suspected of having or with confirmed COVID-19 in order to protect patients, the public, emergency physicians, and other health care professionals.1 Some hospitals and health systems have been unable to supply PPE to adequately meet demand, and others have resorted to reusing PPE in ways that previously would not have been considered, such as sanitizing N-95 respirators for reuse. Individual hospitals and health systems have developed different and changing standards for PPE use, most notably face masks, as well as guidance on what to do if you are exposed with or without proper PPE (see Figure 1). On March 20, 2020, as the extent of infections became more evident, ACEP recommended “health care workers working in the emergency department and EMS should consider wearing a surgical mask all day unless it becomes soiled.”2 As more is learned about COVID-19, including infection rates among health care professionals, PPE best practices are evolving, with use of the previously recommended surgical masks being called into question.3
Figure 1: Sample PPE and Exposure Recommendations (click to enlarge)
Reprinted with permission from the SUNY-Upstate Medical University Hospital Chief Medical Officer’s COVID-19 Report April 7, 2020.
Institutional Responsibilities
At various points throughout this pandemic, emergency physicians, nurses, and other front-line health care professionals were restricted from using PPE brought from home, and others were threatened with termination of employment for raising concerns about PPE.4 If a hospital cannot provide PPE, emergency physicians should be permitted to wear PPE that they have secured for themselves. Effective conflict resolution strategies should be employed if there is disagreement about personal protection and providers should feel safe to speak up about their concerns.
Emergency physicians have a duty to protect themselves, their families, and their communities. In fulfilling these duties, emergency physicians should wear at least the minimum level of appropriate PPE. Emergency physicians should be permitted to wear additional PPE based on individual circumstances, such as pre-existing health conditions, local infection rates, and the clinical context of patient care. These decisions should be made based on the available evidence. Cost and availability should not influence what is considered effective and recommended. Just because supplying N95s can be challenging or expensive does not mean that it should not be done.
Institutional policies should be made with the input and approval of the emergency providers who are assuming the risks. As an invaluable health care resource, emergency physicians must follow an ethical course that is paved by personal protection, not born of selfishness, but rather of the recognition that we must remain stewards of ourselves in order to serve others. Emergency physicians represent a central component of the public health response to COVID-19. If emergency physicians are lost to illness or death, we can no longer contribute professionally and the overall public good, leaving society more vulnerable to COVID-19. The evidence is clear: PPE works and improper PPE can be dangerous.5,6
Responsibilities of Emergency Physicians
Emergency physicians have taken an oath to care for patients, including an assumption of some level of personal risk to themselves. They should, therefore, continue to care for patients as an obligation.7 Emergency physicians are required to report to work unless they are unable to perform their duties, perhaps because of illness, or when the risks to their personal health and safety outweigh the good that they provide. They must take appropriate precautions in order to prevent themselves from being vectors of infectious diseases. Risks of exposure to and infection with COVID-19 is particularly relevant to emergency physicians and other front-line health care professionals, especially given the dynamic nature of the pandemic and the recently reported high rates of asymptomatic COVID-19 positivity.8–10 The unique knowledge, skills, and abilities of emergency physicians, from the understanding of systems of care, the development and interpretation of scientific literature, and bedside clinical care are essential during a pandemic. If an emergency physician becomes infected or ill, a highly skilled professional can no longer provide a fundamental public service. Health care professionals and teams have a responsibility to limit collective exposure by limiting interactions with infected or potentially infected patients and using additional protective barriers when possible. The stewardship of limited PPE is important, and emergency physicians have a right to appropriate PPE as well as a responsibility for prudent stewardship of this limited resource.
Duty is Dependent on PPE Access
Duty and safety should not be at odds, but unfortunately there may be times when emergency physicians must face these morally distressing situations. The emergency physician’s duty to care for patients is dependent on our right to a measure of safety, including the right to access and use of appropriate PPE. We remain one of the few professions that continue to run toward a burning building, and we must be equipped with the necessary equipment to fight the fire. Emergency physicians endure enough threats over which they have limited control, be they physical, legal, or administrative. The threat of contagion from inadequate PPE serves neither the patient nor the public and must be addressed forthwith.
References
- Verbeek JH, Ijaz S, Mischke C, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2016;4:CD011621.
- American College of Emergency Physicians. ACEP’s Position on PPE Use. (updated March 25, 2020). Available at: https://www.acep.org/corona/covid-19-alert/covid-19-articles/aceps-position-on-ppe-use/. Accessed June 30, 2020.
- Luthra S, Jewett C. Widely used surgical masks are putting health care workers at serious risk. Kaiser Health News. Available at: https://khn.org/news/widely-used-surgical-masks-are-putting-health-care-workers-at-serious-risk/ Accessed June 30, 2020.
- Judd, R. ER doctor who criticized Bellingham hospital’s coronavirus protections has been fired. Seattle Times. Available at: https://www.seattletimes.com/seattle-news/health/er-doctor-who-criticized-bellingham-hospitals-coronavirus-protections-has-been-fired/ Accessed April 22, 2020.
- Ong SWX, Tan YK, Sutjipto S, et al. Absence of contamination of personal protective equipment (PPE) by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Infect Control Hosp Epidemiol. 2020;41(5):614-616.
- Kalil L. Nurses at St. Joseph’s blame hospital procedural change for 6 nurses testing positive. CNY Central. Available at: https://cnycentral.com/news/coronavirus/nurses-at-st-josephs-blame-hospital-procedural-change-for-6-nurses-testing-positive Accessed June 30, 2020.
- American College of Emergency Physicians. Code of Ethics for Emergency Physicians. Available at: https://www.acep.org/globalassets/new-pdfs/policy-statements/code-of-ethics-for-emergency-physicians.pdf Accessed June 30, 2020.
- Sutton D, Fuchs K, D’Alton M, Goffman D. Universal Screening for SARS-CoV-2 in Women Admitted for Delivery. N Engl J Med. 2020;382(22):2163-2164.
- Gudbjartsson DF, Helgason A, Jonsson H, et al. Spread of SARS-CoV-2 in the Icelandic Population. N Engl J Med. 2020;382(24):2302-2315.
- Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 Infection in Residents of a Large Homeless Shelter in Boston [published online ahead of print, 2020 Apr 27]. JAMA. 2020;323(21):2191-2192.
Dr. Kraus an emergency medicine physician at Geisinger Health System in Danville, Pennsylvania.
Dr. McGrath is an emergency physician at Seattle Emergency Physicians, Swedish First Hill in Seattle, Washington.
Dr. Brenner is associate professor of emergency medicine at Upstate Community Hospital in Syracuse, New York.
Dr. Vearrier is an emergency medicine physician at the University of Mississippi Medical Center in Jackson.
Dr. Larkin is an ethicist and professor of emergency medicine at Northeast Ohio Medical University, Summa Health in Akron.
Pages: 1 2 | Multi-Page





No Responses to “Emergency Physicians’ Rights and Responsibilities During the COVID-19 Pandemic”