Despite the United States encompassing just 5 percent of the world’s population, it accounts for 84 percent of oxycodone (Oxycontin) and a whopping 99 percent of hydrocodone (Vicodin, Lortab) global consumption. Unfortunately, the prescription opiate epidemic is worsening.
Explore This Issue
ACEP Now: Vol 33 – No 06 – June 2014New, Controversial Opioid Option
Since March 2014, patients and physicians have had a new option with a hydrocodone tablet, Zohydro ER (hydrocodone bitartrate). Hydrocodone (Zohydro ER’s sole ingredient) is one of the most frequently prescribed and, unfortunately, abused opioids. One of the advantages of Zohydro ER is that the relief, or high, can last up to 12 hours per dose.1 Zohydro ER is specifically indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate. Following Zohydro ER ingestion in premarketing studies, hydrocodone levels peak in five to six hours.
According to the package insert, the starting dose for patients who are not opioid tolerant is Zohydro ER 10 mg orally every 12 hours; this is the lowest dose. The package insert defines patients who are opioid tolerant (the target population) as those receiving, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl per hour, 30 mg oral oxycodone per day, 8 mg oral hydromorphone per day, 25 mg oral oxymorphone per day, or an equianalgesic dose of another opioid.2
The presumed benefit of Zohydro ER—other than its strength—is that it doesn’t contain acetaminophen, as do Vicodin and Percocet. It’s on this basis that its maker, Zogenix, has argued that it’s safer than the alternatives. Currently, there are other opiate painkillers on the market that don’t contain acetaminophen. Current recommendations to minimize any risk of hepatotoxicity following chronic acetaminophen use resulted in the Food and Drug Administration recommending reducing the daily dose from 4 grams to 3 grams daily.
According to the Centers for Disease Control and Prevention, prescription opioid deaths have more than quadrupled since 1999. There were 4,030 deaths involving the drugs in 1999, compared with 16,651 in 2010. Therefore, why would the FDA approve Zohydro ER? A better question is, how they could not? If a drug meets FDA requirements, it must be approved if similar drugs have been approved. Zohydro ER could not be scapegoated simply by virtue of being an opioid or for the “sins” of other opiates. Of the Zohydro ER approval process, Bob Rappaport, MD, director of the FDA’s Division of Anesthesia, Analgesia, and Addiction Products, said, “We are obligated at the agency to operate within the regulatory framework, and that includes providing a level playing field for industry. We don’t have a choice by that. It’s the law.”3
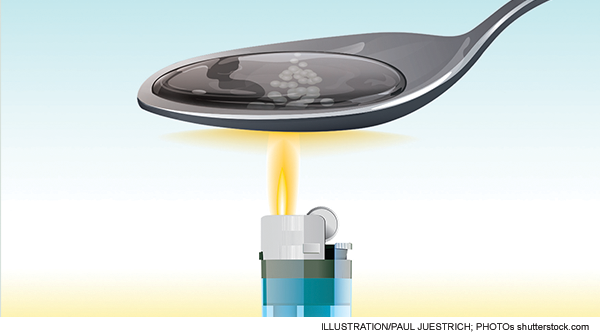
Zohydro ER has been heavily criticized for lacking safeguards that would diminish abuse potential. In its current form, Zohydro ER can be easily crushed, snorted, or injected. Zohydro ER is only currently available in capsule form; hence, it can easily be opened, making pure hydrocodone available. Critics of the drug’s approval suggest that it should have included an “abuse-deterrent” formulation, such as additives like naloxone or niacin that cause unwanted side effects when the drug is snorted or injected but are tolerable when taken orally as prescribed. Zohydro ER does not contain any ingredients that would safeguard against abuse. In the companies’ defense, these additives seem logical but have not been a proven deterrent to abuse.
Purdue Pharma, the maker of Oxycontin, has completed testing of an abuse-resistant version of the painkiller hydrocodone. Purdue Pharma says it plans to submit its extended-release hydrocodone drug to the FDA in late 2014. It will be interesting to see if clinicians adopt this potentially safer formulation.4
What’s a Physician to Do?
As a practicing toxicologist, I err on the side of caution with adopting newer potent opiates. For example, this drug is potentially so potent that an opiate-naive patient could die of an overdose from just two to four pills and a toddler from one capsule. Following overdose or accidental ingestion, it is prudent for patients to undergo an extended observation period. In my opinion, such patients should be observed at least 12 hours, assuming no naloxone was used, until future data are collected.
In summary, the FDA approved Zohydro ER for the management of pain severe enough to require daily, around-the-clock long-term opioid treatment and for which alternative treatment options are inadequate. At least initially, if you prescribe this drug, be aware of this indication. Be aware that the peak may not occur for six hours in “normal” patients in “ideal” circumstances. Be aware that Zohydro ER is metabolized via P450 interactions P450 3A4, and drugs such as macrolides or azole antifungals that inhibit this cytochrome may increase hydrocodone levels. Be aware that ethanol and other CNS depressants potentiate the effect. Be aware that clearance is altered, namely decreased in patients with hepatic and renal disease (not further identified). An FDA-approved patient medication guide, which is available with the product information and can be accessed at www.fda.gov/downloads/Drugs/DrugSafety/UCM374009.pdf, must be dispensed with this medication. Currently, it is approved as a Schedule II drug and can only be dispensed through a physician’s written prescription, and no refills are allowed. There are also stringent recordkeeping, reporting, and physical security requirements for Schedule II controlled substances. Considering the risk-benefit ratio, is this too much to be aware of for one drug?
Patients and physicians want better pain relief and improved patient satisfaction. Mandates warrant “significant decreases in pain scores,” further increasing the demand for a drug such as Zohydro ER. Logically, drug companies will increase supply based on demand. Regulations, lobbying, restrictions, and patient and physician education may decrease the demand for opioids. As individuals, and hopefully as a group, the simplest way for us to decrease demand for Zohydro ER and similar products is not to prescribe them. In conclusion, until further data are available—especially addressing post-marketing safety—it is best to “say no to Zohydo” in the ED.
Dr. LoVecchio is vice chair and research director at the Maricopa Medical Center in Phoenix, professor of emergency medicine, pharmacology, and medicine at the University of Arizona College of Medicine in Tucson, and co–medical director of the Banner Good Samaritan Poison & Drug Information Center.
References
- Rauck RL, Nalamachu S, Wild JE, et al. Single-entity hydrocodone extended-release capsules in opioid-tolerant subjects with moderate-to-severe chronic low back pain: a randomized double-blind, placebo-controlled study. Pain Med. 2014 Feb 12. [Epub ahead of print]
- Zohydro ER package insert. Zogenix Web site. Available at: www.zogenix.com/pdf/ZohydroER_PI_FINAL_102513.pdf. Accessed May 12, 2014.
- Ramin CJ. Why did the F.D.A. approve a new pain drug? The New Yorker. Dec. 3, 2013. Available at: http://www.newyorker.com/online/blogs/currency/2013/12/zohydro-why-did-the-fda-approve-a-new-pain-drug.html. Accessed May 12, 2014.
- Associated Press. Abuse-resistant hydrocodone could sink sales of new drug. New York Times. March 12, 2014. Available at: www.nytimes.com/2014/03/13/business/abuse-resistant-hydrocodone-could-sink-sales-of-new-drug.html?src=recg&_r=0. Accessed May 12, 2014.
Pages: 1 2 3 | Multi-Page




One Response to “Emergency Physicians Urged Not to Prescribe New Opioid, Zohydro ER, Given High Potential for Abuse”
March 27, 2019
DavidDoctors need to be aware of a patient’s true need for an Opioid drug. They need more training to determine a patient’s potential for abuse.