During your busy shift, you get a call that a 27-year-old G3 P2 female who is 28 weeks pregnant has been involved in a motor vehicle collision. She was the restrained driver in a front-end 25-mile-per-hour collision with airbag deployment. The obstetrician-gynecologist team has tasked you with “clearing” the patient from a trauma perspective before she comes to the labor and delivery floor for monitoring. She complains of some abdominal discomfort. On exam, she has no seatbelt sign. You reach for your trusty ultrasound machine to perform a focused sonography for trauma (FAST) exam and obtain all the necessary views. Then you ask yourself, is the FAST exam even applicable in pregnancy?
Explore This Issue
ACEP Now: Vol 39 – No 01 – January 2020Background
Trauma is a leading cause of nonobstetric maternal mortality and affects up to 7 percent of all pregnancies. Both major and minor trauma increase the risk of a pregnancy loss, but pregnant trauma patients are more likely to sustain serious abdominal injuries than nonpregnant trauma patients. The overall fetal loss rate from trauma is reported to be anywhere from 1 percent to 34 percent.1 The fetal loss rate with penetrating abdominal injuries is far higher, at 73 percent.2,3 Additionally, life-threatening traumatic injuries to a pregnant patient should always be considered a life-threatening condition for the fetus because maternal death almost always results in fetal death.4
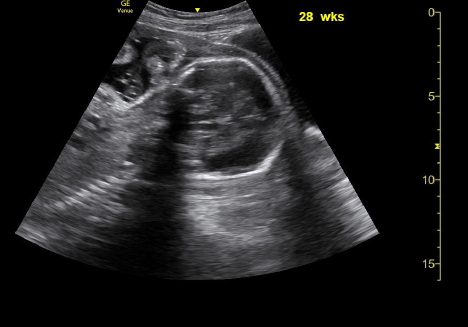
Sagittal and transverse
Because of the risks to both the mother and fetus, emergency and trauma physicians will want to be confident in their physical assessments of pregnant patients with traumatic injuries. Generally, ultrasonography is a preferred imaging modality for this patient population due to lack of radiation exposure. However, the FAST exam, one of the most commonly used assessments to look for free intraperitoneal and pericardial fluid from internal trauma, may be unreliable in pregnant patients.
Limitations of the FAST Exam
The most obvious aspect of the FAST exam that may be different than usual is the pelvic portion of the exam, which can be challenging due to the anatomical changes that accompany pregnancy. Of particular concern is the evaluation of the pouch of Douglas for the presence of hemoperitoneum, which requires special and more advanced ultrasound training than for nonpregnant patients.5
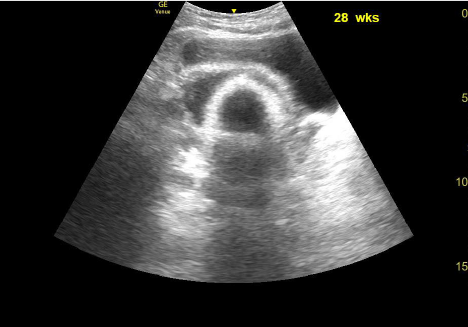
Pelvic ultrasound of a female who is 28 weeks pregnant.
The most common cause of pregnancy loss with nonfatal maternal traumatic injury is placental abruption. This is sometimes assessed during the FAST exam, often when attempting to establish ongoing fetal heart motion, fetal activity, amniotic fluid volume, and gestational age.1,5-7 However, ultrasound is insensitive in diagnosing placental abruption, and a true diagnosis often requires continuous cardiotocographic monitoring.8,9 Furthermore, as in nonpregnant trauma patients, the FAST exam may fail to identify small amounts of intraperitoneal fluid and specific organ injury in pregnant patients.10-14
Pages: 1 2 3 4 | Single Page




No Responses to “Evidence Behind Focused Sonography for Trauma During Pregnancy”