 Our virtual doctors’ lounge, EM Docs, continues to grow! As of the writing of this column, there were 8,292 members—and we’re growing daily, with 365 requests awaiting verification as members add their colleagues and word gets around about our camaraderie!
Our virtual doctors’ lounge, EM Docs, continues to grow! As of the writing of this column, there were 8,292 members—and we’re growing daily, with 365 requests awaiting verification as members add their colleagues and word gets around about our camaraderie!
Explore This Issue
ACEP Now: Vol 35 – No 11 – November 2016There was a time when physicians met in a physical lounge, sat together, chatted about patients and interesting cases, and lifted one another with encouragement both professionally and personally. With the pressures in our current health care system, we find ourselves stretched so thin that we barely have time to spend with our families, much less with time to support one another. Physicians are smart, and we’ve found a way to decrease the stresses by joining together virtually!
Again, in this EM Docs column, I’d like to share some of our most helpful conversations. To maintain the privacy of the group, there won’t be personal attribution or details provided.
Non-Opiate Treatment of Headaches

Figure 1. Many EM Docs are using intranasal lidocaine delivered with a mucosal atomizing device for headaches to avoid opiate use.
As the saying goes, “everything old is new again.” Intranasal lidocaine delivered with a mucosal atomizing device (MAD) is regaining popularity as we search for ways to avoid opiate use in the emergency department (see Figure 1). EM Docs shared both old and new articles for an evidence-based approach to headache treatment.
“Evaluation of Efficacy of Intra-Nasal Lidocaine for Headache Relief in Patients Refer to Emergency Department” is a double-blind, randomized controlled trial studying 90 adult patients with acute headache.1 The dose was one puff of 10 percent lidocaine or normal saline per nostril. After intervention, the mean visual analog scale (VAS) scores were significantly lower in the lidocaine group than the placebo group at 1, 5, 15, and 30 minutes.
Since we lack 10 percent lidocaine in our departments, other (older) articles were referenced including “Intranasal Lidocaine for Treatment of Migraine: A Randomized, Double-Blind, Controlled Trial.”2 In this study, 81 patients with headache were given either a 4 percent solution of intranasal lidocaine or a saline placebo. Fifty-five percent of patients in the lidocaine group had at least a 50 percent reduction of headache compared with 21 percent in the placebo group.
Some EM Docs in the group who had tried this technique used 1 to 1.5 mL per nare with reported success for patients who had failed other treatments.
Recent neurology guidelines for first-step headache treatment are ketorolac 30 mg IV push or 30 to 60 mg intramuscular plus metoclopramide 10 mg IV push over two minutes plus diphenhydramine 25 to 50 mg IV push. Opiates for headaches are not recommended.
When EM Docs were asked about their uses of MADs, their responses included fentanyl, Narcan, Versed, lidocaine for headache, awake intubations and nasopharyngolaryngoscopy, lidocaine with epinephrine or tranexamic acid for epistaxis, and ketamine.
Use Sugar to Reduce Penile Edema
A case report was presented with a patient who arrived with an edematous penis secondary to a metal ring he had placed at the base of his penis. Other EM Docs helped
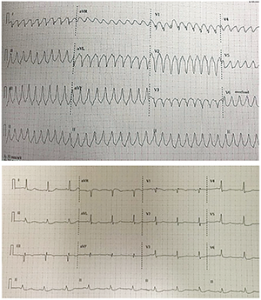
Figure 2. This patient’s elevated aVR was associated with three-vessel disease.
ECGs courtesy of Tony Macasaet, MD, emergency department medical director at Vernon Memorial Healthcare in Viroqua, Wisconsin.
by suggesting a well-documented, but not widely known, “trick of the trade” use of sugar for reduction of edema, similar to the use of sugar for rectal prolapse. Several articles were referenced including “Paraphimosis–Pour Some Sugar On Me.”3 This article described the steps as follows: 1) Mix 50 mL of 50 percent dextrose solution with 2 percent lidocaine jelly, 2) place gauze into the solution, 3) place soaked gauze on the glans of the penis, 4) cover with condom or condom foley, 5) wait one hour, and 6) reduce the paraphimosis.
Another referenced article, “Paraphimosis Treatment & Management,” describes this method: 1) Apply 2% lidocaine gel to the penile skin for a few minutes to an hour before penile manipulation to reduce pain, 2) wrap the penis in plastic and apply ice packs, 3) use compressive elastic dressings, and 4) apply direct circumferential manual compression.
Haldol for Vomiting
Many of the EM Docs discussed successfully relieving vomiting in patients with gastroparesis and cyclic vomiting with doses of Haldol, ranging from 2 to 5 mg IV. Some also add 25 to 50 mg of IV Benadryl. Approximately 50 EM Docs reported using Haldol for vomiting with success on multiple occasions.
“Haloperidol for Treatment of Cannabinoid Hyperemesis” reports a case of cannabinoid hyperemesis syndrome (CHS) and cyclical vomiting where the CHS improved significantly after treatment with haloperidol in the emergency department.5
The dose was one puff of 10 percent lidocaine or normal saline per nostril. After intervention, the mean visual analog scale scores were significantly lower in the lidocaine group than the placebo group at 1, 5, 15, and 30 minutes.
Pay Attention to aVR
The patient with the ECGs in Figure 2 presented talking, then became unresponsive with pulseless ventricular tachycardia, was cardioverted, woke up, and had the second ECG performed. He was sent for catheterization and had critical left main stenosis and severe three-vessel disease.
Dr. Smith’s ECG Blog has an excellent discussion on the clinical significance of augmented vector right (aVR) elevation:6
“Ischemic ST elevation in aVR occurs in two broad categories: 1) in patients with recognized STEMI (due to coronary occlusion, usually of the LAD) and is associated with higher mortality than in patients without STE in aVR and 2) in patients without ischemic ST elevation, in which case there is always diffuse ST depression of subendocardial ischemia (which can be due to supply-demand mismatch or due to ACS). If due to ACS, this STE in aVR is associated not only with acute LM insufficiency, but alternatively with 3 vessel disease, or with LAD insufficiency.”
EM Docs continue to use crowdsourcing to improve patient care in real time as well as to prevent burnout by supporting one another with camaraderie. Emergency physicians can’t always share their challenges with their non-physician family members. EM Docs allows for true understanding of the bedside challenges that are unique to our profession.
 Dr. Moody, founder of the EM Docs Facebook group, is president of the Tennessee College of Emergency Physicians and former emergency department chair for Mountain States Health Alliance.
Dr. Moody, founder of the EM Docs Facebook group, is president of the Tennessee College of Emergency Physicians and former emergency department chair for Mountain States Health Alliance.
References
- Mohammadkarimi N, Jafari M, Mellat A, et al. Evaluation of efficacy of intra-nasal lidocaine for headache relief in patients refer to emergency department. J Res Med Sci. 2014;19(4):331-335.
- Maizels M, Scott B, Cohen W, et al. Intranasal lidocaine for treatment of migraine: a randomized, double-blind, controlled trial. JAMA. 1996;276(4):319-321.
- Fu J, Watts M, Coralic Z. Trick of the trade: paraphimosis–pour some sugar on me. Academic Life in Emergency Medicine website. Accessed Oct. 24, 2016.
- Brooks NA, Brown JA. Paraphimosis treatment & management. Medscape website. Accessed Oct. 24, 2016.
- Hickey JL, Witsil JC, Mycyk MB. Haloperidol for treatment of cannabinoid hyperemesis syndrome. Am J Emerg Med. 2013;31(6):1003.e5-6.
- Smith SW. ST Elevation in lead aVR, with diffuse ST depression, does not represent left main occlusion. Dr. Smith’s ECG Blog website. Accessed Oct. 24, 2016.
Pages: 1 2 3 | Multi-Page



No Responses to “Facebook Group, EM Docs, Support Emergency Physicians in Practice”