Editors’ Note: This article was accepted on March 13, 2020, and was accurate at that time. Because information about SARS-CoV-2 and COVID-19 is evolving rapidly, please verify these recommendations and information.
Explore This Issue
ACEP Now: Vol 39 – No 04 – April 2020Over the course of these past several weeks, our area hospitals have been crafting a set of rapidly evolving protocols to combat the spread of SARS-CoV-2, the novel coronavirus that causes COVID-19, and develop best practices to care for our COVID-19 patients.
Since the outbreak began, our colleagues locally and nationally have been reaching out to us for assistance as they start to see cases. We hope that by sharing our work, we can assist your teams and facilities to prepare and move more quickly.
Though protocols are frequently being revised as we learn more, there are several ways to ready your emergency departments for these patients. These include creative approaches to staff training, improvements in the physical space for isolation capacity, equipment to procure/inventory, and systems for providing patient care to minimize staff exposure.
We hope you can benefit from these recommendations while you have the time to prepare yourselves and your departments. The most important and time-critical component of COVID-19 response protocol is communication.
Consider Activating Your Incident Command System
Your incident command system should include communication early and often between emergency departments, hospitalist services, ICUs, local and state departments of health (DOHs), emergency medicine services (EMS), leads, and outreach leads to vulnerable populations (eg, local skilled nursing facilities [SNFs], jails, homeless shelters). In our experience, SNFs have been particularly vulnerable and have been the source of most patients and fatalities.
Developing communication links with local SNFs for the purpose of creating a transportation and hospital disposition plan prevents proximately located hospitals from being overwhelmed by a single SNF experiencing an outbreak.
The following cheat sheet is in the staff/stuff/space/systems format of simple ideas to consider for preparing.
Staff
Initiation of Staff Preparations
Fit testing for airborne precautions should be up-to-date within the last month for all staff, including radiology, maintenance, housekeeping, and other ancillary staff. Every physician and nurse should attest to watching the proper donning/doffing technique recommended by the Centers for Disease Control and Prevention (CDC) in the links in the “Resources” sidebar, and in-person training should be considered.
Staff should update their own home personal safety plans, including creating backup child care plans and stocking household supplies so that when work gets busy, their home plans and supplies are ready and they can concentrate on work.
Communication
Incident command structure should be followed, with centralized communication, messaging, and task delegation, including:
- Identify a liaison to communicate regularly with the local DOH.
- Identify a liaison for communications with the media.
- Identify a COVID-19 hospitalist lead for admissions that are not to the ICU and an intensivist lead for those to the ICU.
- Identify outreach leads for EMS, the homeless and shelter community, SNFs, and jails if your hospital receives these patients.
Stuff
Inventory current amounts of sanitation supplies (especially alcohol-based hand gel and bleach wipes); pulse oximeters; masks, powered air-purifying respirators (PAPRs), and shrouds for PAPR; mirrors for doffing stations; and disposable stethoscopes to anticipate increased needs. We have run short of flu swabs and personal protective equipment (PPE). Consider storing these supplies in ways that prevent hospital personnel and guests from removing them for personal use.
Assess supplies of key medications including antibiotics, sedation, analgesia, neuromuscular blockade, and crystalloid. Plan for use of metered dose inhalers with spacers instead of nebulizers to reduce infectivity.
Establish protocols for handling patient specimens (blood, urine, respiratory viral testing, etc.).
Hospitals should determine how many ventilators are available, including noninvasive positive pressure devices and anesthesia machines; reach out to ambulatory surgery centers for the possibility of using anesthesia machines; and assess the number of extracorporeal life support pumps and circuits available.
Space
Develop a department plan designating which areas of the emergency department will be dedicated to droplet precautions and which areas are negative pressure rooms appropriate to airborne precautions. For areas without an antechamber, consider creating a taped “warm zone” outside of the room for proper doffing. Ensure donning/doffing stations are set up with all needed supplies. Consider taking a photo of the station to post to ensure proper setup. How will you secure these supplies (especially the hand gel and wipes)?
Consider cohorting patients with mild illness who are “patients under investigation” in internal waiting rooms away from well patients or those who could be immunocompromised.
Use phones in the patient rooms to interview noncritically ill patients to reduce trips in and out of the room and to coordinate with nursing or respiratory therapy when they are at the bedside.
Movements
Consider how patients will be transported from the waiting room through the emergency department to the isolation or precautions room. What route will they take to minimize exposure from the emergency department to the floor or unit dedicated within your hospital?
What route will patients take from the emergency department to the inpatient unit? Use security to facilitate clearing the route, hold the elevator, and ensure that the elevator is cleaned after patient transport.
What route will your used supplies take to be cleaned, and how will your nasal swabs be transported to the lab (eg, we are not using our tube system)?
Diagnostics
Develop plans for terminal cleaning of CT scan rooms and other bedside diagnostic equipment (portable radiology, ultrasound, etc.). For example, will you have a dedicated ultrasound?
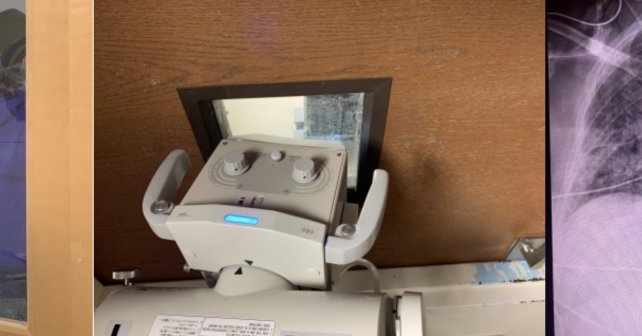
We have developed a process to perform portable radiographs through the door window for patients in isolation, reducing risk to staff and the need to clean portable units (see Figure 1). The radiographs have been found to be of acceptable quality for reading using this technique.

Figure 1: Radiology teams from our institution have minimized staff and equipment exposure by performing single-view portable radiographs through the windows on doors to isolation rooms. Left: The patient is positioned standing or sitting in front of the door inside the isolation room with a nurse/staff wearing a lead shield, holding the plate to the patient’s chest. Center: The portable machine camera is brought close to the glass, and adjustments are made to the machine to optimize the film. The film is passed by the gowned nurse outside the room with removal of the plastic sheet while passing to the X-ray staff outside the room, keeping the plate clean. Right: While artifact from the window is sometimes present on the film, our radiologists have been able to read from these for multi-focal pneumonia and tube placement.
Credit: University of Washington
Systems
Staffing
Plan to have a double backup system in place ensuring that if staff members are sick, there is an easy system to call in relief without having to scramble. This system also protects against staff members feeling remorse or hesitance about calling in sick and contributing to dangerous “presenteeism” and coming to work sick.
Consider:
- Canceling communal food in meetings and care areas and moving to tele-education and online meetings.
- Updating staff flu shots.
- Requiring use of scrubs instead of wearing personal clothes to work and encouraging minimization of jewelry and personal items as fomites.
- Using gel-in/gel-out hand hygiene and redoubling efforts to ensure 100 percent compliance for all patients.
- Creating a hospital-wide plan for backup child care so physicians, nurses, and other staff are not staying home to care for their children if schools close.

Figure 2: Physicians practice intubating using the glidescope while in a PAPR with a shroud.
Credit: University of Washington
Training
Arrange in-person donning/doffing training by “supertrainers” for all ED staff. Once an airway plan has been established, use simulation training to get staff comfortable with new procedures and protocols (eg, intubating using the glidescope while in a PAPR with a shroud, as shown in Figure 2).
Tracking Systems
Review the current system or create a new one for tracking exposures and symptoms when a COVID-19 exposure happens for staff or when staff members are sick. For example, when will they return to work, and how will they get their test results?
Intubation and Airway Algorithms
Review plans for limiting staff exposure to aerosolization of COVID-19. Consider not using high-flow nasal cannula or noninvasive positive pressure ventilation in the emergency department unless adequate airborne isolation can be guaranteed and limiting use of nebulized medication. Intubation should occur only by those trained in how to intubate while in a PAPR with shroud. Follow a COVID-19-specific protocol for intubation developed by your hospital’s airway leads.
Consider PPE use, use of video laryngoscopy, premade medical airway bags, reentry and intubation checklists, and rapid sequence intubation to decrease aerosolization of particles with bag-valve masks.
Review methods for addressing severe hypoxemia and acute respiratory distress syndrome (ARDS) with ventilation, medication, and other maneuvers with all staff (eg, titration positive end-expiratory pressure, neuromuscular blockade, recruitment maneuvers, and proning).
Bundle Care
Plan ahead for blood draws, ECGs, and medication administration to minimize trips into and out of the patient’s room. Build kits with preassembled supplies to be used in isolation areas. Establish protocols for testing patients in conjunction with your lab’s ability to run these tests.
Create scripts for 911 call centers to ask about COVID-19 risk factors before sending EMS to a scene. Develop scripts for your transfer center to use screening questions regarding symptoms and COVID-19 status with the goal of identifying potential COVID-19 patients prior to ED arrival. Have EMS call ahead to alert emergency department to high-risk COVID-19 patients from the field. Draft outward-facing documents with clear instructions for the community to call their doctor prior to coming to the emergency department to reduce overcrowding.
Interfacility Triage
If your center is a receiving center for stroke or other transfers, ensure that there are COVID-19 screening questions being asked by all accepting physicians and services.
Extracorporeal Membrane Oxygenation (ECMO)
Consider risks and benefits of citywide and regional referral of patients to ECMO centers. Risks of transport may include disease spread, risk to transport personnel, and overwhelming ECMO centers’ general ICU resources. Develop strict criteria for ECMO initiation only to those with the highest chance of survival given the high number of potential ECMO candidates and limited capacity. If patients require transfer from low-resource hospitals, consider triaging potential ECMO candidate patients (young, otherwise healthy, single organ failure) to large urban ECMO centers. This may decrease the frequency of patient transports for eventual ECMO referral.
Consider how mobile ECMO retrieval teams may be used to maximize ICU care at referral facilities. Once patients have failed conventional hypoxemia therapies, they will be too unstable for transport without ECMO. Coordinate with neighboring ECMO centers to exchange experience and knowledge, and potentially develop care guidelines for this patient population.
Intubation and Respiratory Support
Personnel from critical care, respiratory therapy, and anesthesiology should convene to develop approaches to support for suspected or confirmed COVID-19 patients with respiratory failure. Controversy exists about the use of noninvasive positive pressure ventilation and high-flow nasal cannula, which may disperse secretions and therefore virus.
We have opted to perform early tracheal intubation for these patients with placement on mechanical ventilation with a viral filter. Intubation should occur ideally in negative pressure rooms using airborne precautions.
- The intubating clinician should use a PAPR with shroud and follow donning/doffing procedures.
- Additional staff should be minimized (ideally, one nurse and one respiratory therapist).
- We favor the use of video laryngoscopy to increase the distance between the intubating clinician and patient’s aerodigestive tract along with the rapid sequence intubation technique to minimize coughing or dispersion of secretions during bag-mask ventilation.
- Viral filters can be placed in-line with bag-valve masks.
- If sidestreamwaveform capnography devices are used, make sure a viral filter is placed in-line proximal to the end-tidal CO2 adapter (ie, directly on the end of the endotracheal tube, mask, or laryngeal mask airway). Otherwise, contaminated secretions may theoretically leak into the end-tidal CO2 tubing and perhaps back to the monitoring module.
Code Blue/Clinical Emergency Response
A dedicated plan for response to clinical emergencies should be created for patients with suspected or confirmed COVID-19. The plan should include limiting responding personnel, ensuring isolation precautions are maintained, and limiting aerosolizing procedure.
Consider appointing a dedicated isolation “captain” to ensure only essential staff enter the room, appropriate PPE are used, and equipment is decontaminated appropriately. The plan should include early discussions about “do not resuscitate” status with next of kin for critically ill infected patients.
The authors are in the department of emergency medicine at the University of Washington, Harborview Medical Center in Seattle.




No Responses to “Get Your Emergency Department Ready for COVID-19”