Hasbro Children’s Hospital (HCH) is a busy pediatric hospital in Providence, Rhode Island, and a teaching hospital for the Brown University School of Medicine. Part of the Lifespan Health System, it is staffed by physicians from the University Emergency Medicine Foundation (UEMF), which is dedicated to running operationally sound and efficient emergency departments. The emergency department treats 52,000 patients a year in its 36 beds. The leadership team was looking to re-engineer patient flow and workflow to become more efficient. It had been on a journey to improve wait times and performance metrics.
In March 2014, the emergency department reported wait times to see a clinician of 72.4 minutes, something anxious parents regularly complained about. The emergency department began a number of improvement initiatives including a “pull to full” project, which traded a lengthy traditional triage process for a quick-look triage and bedside triage and registration process. The results were very promising and wait times were cut in half. However, the ED leaders—Frank Overly, MD, medical director; and Lynn Pittsinger, RN, nursing director—wanted to do more. The department was struggling to efficiently manage low acuity patients and a growing behavioral health (BH) burden. Together, the leadership formed a highly functional improvement team that included physicians—Laura Chapman, MD, Linda Brown, MD, and Elizabeth Jacobs, MD—nurses—Samantha Leary, Maureen O’Neill-Britt, Stacy Schindle—and a data analyst, Dennis Ferrante. This team developed an ambitious group of changes and prepared for implementation. The project was dubbed “Expedite to Excellence” or E2, and this appeared on posters and emails sent to staff.
A few things to note about pediatric emergency medicine patients:
- Children have a lower rate of being admitted (10.4 percent according to the most recent Emergency Department Benchmarking Alliance survey), equating to a possible shorter length of stay (LOS).
- Pediatric patients have a greater need for procedural sedation. This has implications for space and staff and for what conditions might be treated in a fast track setting.
- Even blood draws or IV placement can be a two- or three-person task, especially in younger patients who may need staff to hold them still for these procedures. This has staffing implications (ie, more certified nursing assistant or tech support).
- Pediatric volumes are lower on mid-week days and in the summer months and higher on Mondays and Sundays, which has more staffing and patient flow implications.
- Pediatric BH complaints are on the rise and these patients have longer LOS. This affects bed utilization and has a de facto “boarding” effect.
The Hasbro leadership set out to right or remedy its flow problems. It decided that instead of tinkering with small changes, they would implement a “change package” with a number of initiatives that would go live all at once. The change package included the following improvements:
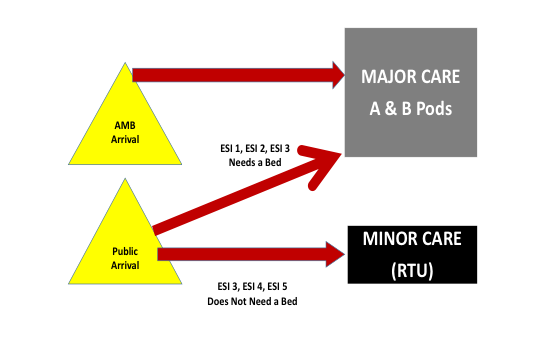
- Design and Standardize the Flow Model: Conceptually, the leadership supported a flow model that streamed patients to geographic areas according to their acuity and anticipated resource utilization. The model is depicted in Figure 1, and part of the implementation included flow standardization and keeping the model clinician independent.
- Build Out A Low Acuity Service Line: The rapid treatment unit (RTU) concept is being adopted around the country (see Figure 2). It provides a place to see and treat lower acuity patients (both fast track and minor illness patients) often without the patient occupying a bed in a room. Though almost a third of patients seen in HCH are low acuity, there was no specific service line for these patients until 6 p.m., when the staff would migrate to the empty clinic in the basement. As a result, low acuity patients experienced long waits to see clinicians.
- Close C Pod (the Lower Level): The C pod, in the basement, was wildly inefficient and would see only 18 patients a day in its 10 beds. The logistics made this remote site run inefficiently as patients and staff had to make many trips up and down stairs for imaging and supplies. The location made it a barrier to smooth patient flow and not an asset for the department. Still, the staff felt it was a safety valve for the department and initially were resistant to the idea of giving it up. The project involved ceasing to move patients into the space downstairs, which was not optimized and did not provide returns on the current resource investments.
- BH Improvements: The department was struggling with the management of BH patients who often experienced delays. The HCH leadership team articulated a new flow of BH patients with early medical clearance (medical clearance of pediatric BH patients is very brief) and cohorting of these patients in a special area of the department.
The results of the change package have impressed the hospital leadership, the stakeholders, and the community (see Table 1).
The “door-to-doc” times, which had been cut in half with the “Pull to Full” initiative, were reduced even further with the change package. These wait times are settling in at under 20 minutes, something that is hard to do without putting a physician in triage. The overall LOS has come down, particularly the LOS of the RTU, which is consistently well under the 90 minutes goal that was set. The left-without-being-seen rate is now averaging less than 0.5 percent, down from 1.41 percent. Further, the RTU is managing 18 percent of the volume, or 26 patients per day in five treatment spaces. While low acuity patients spent more than two hours in the lower level C Pod, they are now typically in and out in just over one hour.
The wait times to see a clinician for BH patients have been reduced by 40 percent, another win for the team (see Table 2).
The team started using Tableau, a software platform for tracking data that allows for daily analysis of ED operations. One of the nice features in Tableau is called the “temperature gauge,” which allows a quick visual of performance (see Figure 3).
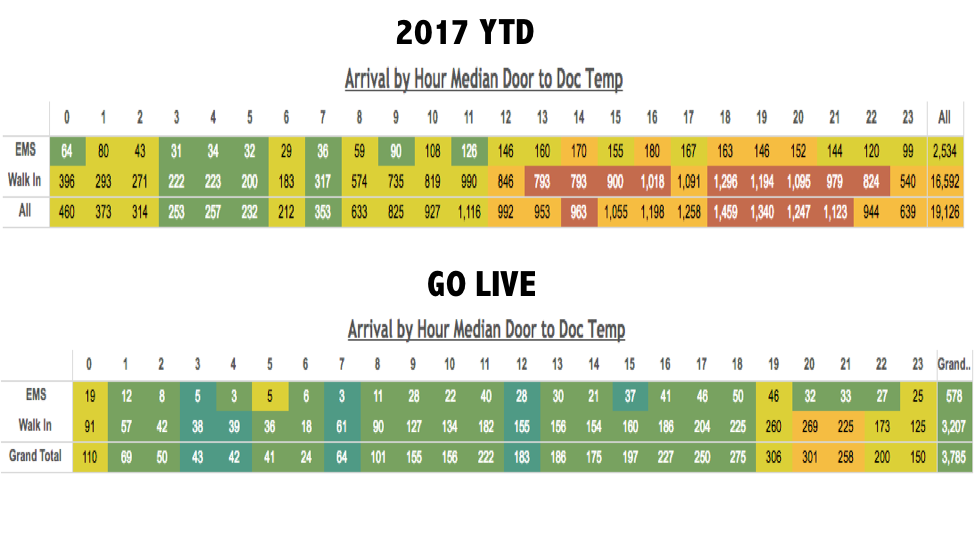
Figure 3: Tableau temperature gauges for before (top gauge) and after (bottom gauge) implementation of Hasbro Children’s Hospital’s change package. Arrivals are mapped by hour, with the the top row of the gauge indicating EMS arrivals, the middle row ambulatory patients, and the bottom row total patients. Patients waiting under 30 minutes are green, and patients waiting more than an hour are red. Before the change package (top guage), the wait times to see the physician were 39 minutes, and the red indicates that some hours of the day some patients waited more than an hour. The lower temperature gauge shows the median wait times by hour after the new change package went live.
The HCH leadership team lived up to their project slogan “Expedite to Excellence.” And according to the Figure 3, the team has definitely gone green!
Pages: 1 2 3 | Multi-Page









No Responses to “Hasbro Children’s Hospital’s “Expedite to Excellence” Project Improve Wait Times and Performance Metrics”