
COVID-19 has infected more than 247 million people worldwide, leading to over 5 million deaths.1 Distribution of critically ill patients to available critical care units and tertiary centers for specialized care has been an essential strategy to maximize health system resources. These circumstances have put a strain on and created unique needs for air medical transport in the United States.
Explore This Issue
ACEP Now: Vol 40 – No 12 – December 2021STAT MedEvac is a regional critical care transport network serving a catchment area of roughly 4 million people. Affiliated with the University of Pittsburgh Medical Center, STAT MedEvac transports 13,000 patients per year, operating 18 base sites serving five states and the District of Columbia. Since March 2020, we have developed and refined comprehensive procedures to address the clinical needs posed by the COVID-19 pandemic and, to date, have transported over 2,000 confirmed or suspected COVID-19 patients.
Clinician Safety and Personal Protective Equipment (PPE)
Early in the pandemic, managing uncertainty regarding transmission, diagnosis, prevention, and treatment called for definitive, dynamic procedures. For real-time education and communication, we implemented weekly systemwide video conferences to discuss current recommendations, answer questions, and facilitate necessary changes. Daily operations calls at shift change addressed more immediate needs.
To reduce on-duty exposure, we established a preshift health assessment. Staff who screened positive were referred to regional management and occupational health. We also enacted universal masking while on duty; instituted daily cleanings; and deployed physical distancing and barriers in our administrative offices, maintenance areas, and communications center.
A three-tiered system identified patient COVID-19 status prior to transport. First, our referral center screened for known infection. Once a transport asset was requested, our communications center performed a second-level screen with the referring facility including symptoms and testing for COVID-19. At bedside, crews performed a third, more thorough screening based on symptoms, lab studies, and clinical assessment to identify patients of interest (PUIs). In accordance with recommendations from the World Health Organization (WHO) and the Air Medical Physician Association (AMPA), personnel used airborne precautions for all PUIs.2

STAT crew at base, ready with PPE.
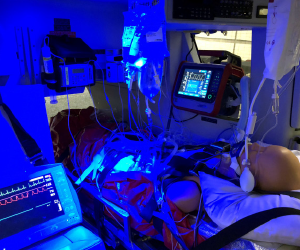
Typical setup inside STAT MedEvac aircraft, featuring a loaded patient on ventilator, multiple infusions, and balloon pump.
During the first wave of COVID-19, we employed a PPE strategy that included surgical masks for all patients and crew, escalating to eyewear, N95 mask, surgical gown, and gloves if the patient met COVID-19 high-risk criteria (including any of the following: positive or pending COVID-19 test, isolation status, close contacts within 21 days, fever absent alternate source, suspected respiratory infection, noninvasive or high-flow ventilation, or need for aerosolizing procedures). We had no known patient-to-staff case transmission during that time. However, the second wave brought an increasing number of COVID-positive patients missed by screening, including trauma and stroke patients from missions where limited history was available. To mitigate unexpected crewmember quarantines, in October 2020, we adjusted our requirements for crew to wear elevated levels of PPE for all patient interactions. To offset supply concerns, N95s were reused per Centers for Disease Control and Prevention recommendations. Additionally, each crewmember was issued a half-face respirator containing removable P100 filters that permitted easy disinfection. To ensure appropriate resource allocation, we tracked PPE stock counts daily at each base and communicated to central management.
Vehicle Logistics
The air medical transport environment (in Airbus EC-135 and EC-145 helicopters) presented a challenge to maintaining isolation precautions because patients and staff were contained in small compartments with unavoidable prolonged exposure (median flight time 19 minutes; interquartile range 13–31 minutes). Because only a cloth divider separates the cockpit and main cabin, even our pilots don N95 masks for all patient transports. To avoid unnecessary exposure, they remain in the cockpit, stay out of patient clinical areas, and do not assist in patient loading or unloading. In the aircraft cabin, outside air ventilation is selected over air recycling.
Following transport of COVID-19 patients or PUIs, aircraft and equipment undergo a regimented decontamination process. All equipment is removed from the aircraft, and the floor of the airframe, the stretcher, and equipment tracks are swept. The entire patient compartment and all equipment are then sprayed with disinfectant (3M’s TB Quat) and allowed to dry. After an appropriate dwell time (minimum 20 minutes), the main cabin is wiped down with antiseptic wipes before returning the equipment. Recently, we adopted the use of an AeroClave fogger for more efficient decontamination.

EC-135 on top of the University of Pittsburgh Medical Center Mercy Hospital helipad.
Clinical Care
Aerosolizing Procedures
Aerosolizing procedures such as intubation, nebulized medications, and noninvasive ventilation (NIV) create the highest risk of virus transmission. Additionally, certain emergent procedures (needle decompression) carry some risk. We limit aerosolizing procedures in the aircraft, performing them prior to transport when possible. We use video laryngoscopy to optimize first-pass success and reduce exposure time. During NIV, we place in-line HEPA filtration and use nonvented masks while monitoring and minimizing leaks. Nebulization and high-flow nasal cannula (HFNC) were initially used on a limited basis; however, more recently with improved protection assurance through PPE and vaccinations, utilization has increased. These interventions have been provided for COVID-19 and other patients, using the highest-level PPE.
Oxygen Consumption
COVID-19 hypoxemic respiratory failure requires massive oxygen delivery consuming up to 80 LPM through NIV and HFNC. Our aircraft are fitted with either one or two M-size main oxygen cylinders (≥1,200 psi) and two portable cylinders (sizes D and E, 2,000 psi). Despite having more than 2,000 L, oxygen remains a limiting factor. Crew training and a custom smartphone application facilitates oxygen consumption calculations prior to transport, supplemented by bedside discussions with a medical director to ensure adequate supply, delivery method, and FiO2 optimization. A minimum 30-minute oxygen reserve is required for safety.
Mechanically Ventilated Patients
Nearly one-quarter of STAT MedEvac transports are mechanically ventilated. Patients presenting with COVID-19–related respiratory failure present unique challenges in transport. To minimize risk to the crew, we use an in-line HEPA viral filter and clamp the endotracheal tube prior to any transitions. Treatment of hypoxemia in intubated patients generally follows the ARDSnet mechanical ventilation protocol.3 We primarily use adaptive support ventilation (ASV) with the Hamilton-T1, a pressure-regulated volume-control mode that automatically adjusts tidal volume and respiratory rate based on a target minute volume, dynamic lung compliance, and the Otis work of breathing equation.4 While this mode has been successful in most COVID-19 patients, some require alternate ventilation strategies.
Prone Positioning
Proning hypoxic COVID-19/acute respiratory distress syndrome (ARDS) patients refractory to other treatments improves pulmonary mechanics and oxygenation.5 We have performed prone transports since 20126 and provided all staff with refresher training using printed and video materials. Patient characteristics for which proning is considered include a P:F <150 despite FiO2 >0.6 and PEEP >10. Self-proning for awake patients is uncommon due to the limited space and aircraft restraint systems.
Extracorporeal Membrane Oxygenation (ECMO)
ECMO may rescue patients with refractory hypoxemia. We provide both primary and secondary ECMO transport. For primary ECMO, we deploy a cannulation team including two physician proceduralists and a perfusionist to outlying facilities to cannulate patients who would otherwise be too ill to transport safely. Secondary transports require only our standard crew and a perfusionist to retrieve a patient already on ECMO. ECMO missions require additional planning, equipment, and time.
Health Resource Management and Telemedicine
Across our health system, we experienced capacity shortages due to both bed space and staffing. Our medical direction and patient referral center work closely together with a COVID-19 resource center for the health system. This system provides teleconsultation to referring hospitals to maximize their ability to care for critically ill COVID patients on-site and to limit transfers for patients who both exceed local resources and might still benefit from quaternary care. As such, we have the unique ability to optimize bed utilization within the regional system, ensuring that destinations are appropriate, and patients are distributed according to available resources.
To conclude, during this global crisis, we found that an adaptive, comprehensive approach to operations and clinical care cultivated a safe and promising experience for our patients and personnel engaged in critical care air medical transport.
Dr. George is a flight physician for STAT MedEvac and chief resident at University of Pittsburgh Emergency Medicine. Dr. Felock is an emergency medicine resident at the University of Pittsburgh. Dr. Guyette is medical director of STAT MedEvac. Dr. Martin-Gill is associate medical director of STAT MedEvac. Dr. Nusbaum is EMS medical director at the University of Pittsburgh Medical Center. Dr. Morris is assistant medical director of STAT MedEvac. Dr. Weiss is assistant medical director of STAT MedEvac and assistant professor of emergency medicine at the University of Pittsburgh School of Medicine.
References
- Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533-534.
- Air Medical Physician Association Board of Trustees. Air Medical Physician Association position statement on COVID-19. Air Med J. 2020;39(3):221.
- Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
- Fernández J, Miguelena D, Mulett H, et al. Adaptive support ventilation: state of the art review. Indian J Crit Care Med. 2013;17(1):16-22.
- Scaramuzzo G, Gamberini L, Tonetti T, et al. Sustained oxygenation improvement after first prone positioning is associated with liberation from mechanical ventilation and mortality in critically ill COVID-19 patients: a cohort study. Ann Intensive Care. 2021;11(1):63.
- DellaVolpe JD, Lovett J, Martin-Gill C, et al. Transport of mechanically ventilated patients in the prone position. Prehosp Emerg Care. 2016;20(5):643-647.
Pages: 1 2 3 | Multi-Page




No Responses to “How One Air Transport Network Adjusted to the COVID-19 Era”