
Editors’ Note: This article was accepted on April 6, 2020, and was accurate at that time. Because information about SARS-CoV-2 and COVID-19 is evolving rapidly, please verify these recommendations and information.
Explore This Issue
ACEP Now: Vol 39 – No 05 – May 2020Here, we will itemize the process that was implemented in our emergency department for high-risk intubations of patients suspected of having SARS-CoV-2, the virus that causes COVID-19. The principal factors in establishing a formal protocol focused on limiting exposure of health care workers and minimizing unnecessary personal protective equipment (PPE) utilization. The major adaptation is the construction and implementation of a protective intubation box in an attempt to reduce circulated viral aerosolized particles during the intubation process.
PPE
Once it is established that the patient will be intubated, the most experienced physician, registered nurse, and respiratory therapist proceed to don PPE. They proceed in this order: small shoe covers, white coverall zip-up suit if available, boot covers, one set of gloves, Tyvek gown, second set of gloves, N95, bouffant cap, neck cover, and face shield (this may be substituted for a hood). Once PPE is in place, they proceed into a negative pressure room with all necessary medications and equipment for the procedure. This should include post-intubation sedation and pain medications.
Setup
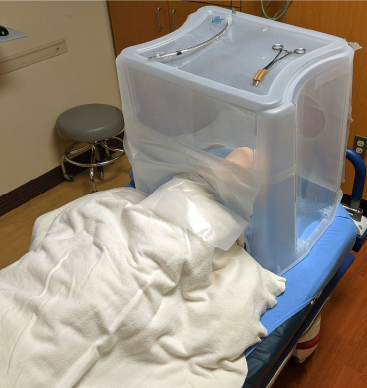
Figure 1 (LEFT): Simulated COVID-19 patient covered by protective intubation box.
Ideally, each individual involved with the intubation should have a counterpart of their discipline outside the room as backup. Place the intubation box over the patient prior to the patient moving to a negative pressure room if they are not already there to decrease viral spread (see Figure 1). Intubation tools may be placed next to the patient’s head prior to placing the protective intubation box or placed through the access hole at the cephalad portion of the box. Necessary tools include: large forceps with protective cover over teeth to clamp the endotracheal tube after confirmed placement, endotracheal tube and stylet with 10-cc syringe attached, and video laryngoscope.
Procedure

Figure 2: Simulated COVID-19 intubation process with protective intubation box.
PHOTOS: David Weech & John Ashurst
Rapid sequence induction medications are administered. The physician then utilizes the two holes to intubate the patient as routinely done (see Figure 2). Once the tube is placed, the stylet is removed and the tube is then clamped with the large forceps, followed by insufflation of the cuff. The options at this point are to remove the intubation box completely as the system is closed or to proceed with the box in place. If the box is kept in place, the nurse passes the ventilator tubing through the caudal aspect of the box and holds the tube in place while a respiratory therapist works through the two primary operator holes to attach the endotracheal tube securing device.
The intubation team then stays in the room for one complete cycle of ambient air, according to local specifications. All necessary related procedures likely to be needed in the near future should be performed at this time to preserve PPE. These may include placement of nasogastric tubes, central lines, arterial lines, chest tubes, etc. The team then moves to the anteroom to doff PPE. This process should be done in a systematic manner: Remove of Tyvek gown and first set of gloves; perform hand hygiene with hand sanitizer; remove the white coverall, boot cover, and second pair of gloves; hand hygiene; place a new set of gloves to remove head covers (including N95); remove of the final pair of gloves; and hand hygiene for a third time. The team may then return to regular duties in the department. Once the patient is transported out of the emergency department, the drapes on the intubation box are discarded. The box is then wiped down with appropriate disinfectant to be reused after the time frame specified by the manufacturer of the disinfectant.
Conclusion
While this rigorous process may seem excessive, we suggest it out of recognition of the severity of the situation we face today. The possibility of losing critical health care workers and medical personnel if they are inadvertently or carelessly exposed to SARS-CoV-2 is far too great to ignore. Emergency departments are among the most critical resources of the health care system. If proper protective measures such as those suggested here are not taken, our ability to save the most lives and to keep the largest number of people healthy will be compromised.
Dr. Weech and Dr. Ashurst are in the department of emergency medicine at Kingman Regional Medical Center in Kingman, Arizona.
Pages: 1 2 3 | Multi-Page




No Responses to “How to Intubate Suspected COVID-19 Patients With a Protective Box”