
A 24-year-old male with history of quadriplegia and traumatic brain injury presents to the emergency department with hemorrhage in his oral cavity and blood from his tracheostomy tube. He has had a tracheostomy for approximately 15 months since his injury. Blood is spurting from the orifice of the tube.
Explore This Issue
ACEP Now: Vol 43 – No 03 – March 2024Tracheo-innominate fistula (TIF) is an unusual and frequently lethal complication of such definitive airway placement. First reported in 1879 in the case of diphtheria in a pediatric patient, TIF is fatal without surgical treatment due to hemorrhage and failure of airway security. It occurs after an estimated 0.1-1 percent of tracheostomies.1,2,3 Unlike most lethal entities, TIF does not predominantly affect the elderly. In one case series of seven patients, the average patient age was 15.7 years, all of whom had prior severe neurological deficits such as cerebral palsy, agenesis of the corpus callosum, or muscular dystrophy.4
Sentinel bleeding may occur in more than 50 percent of patients, with peak incidence of three days to six weeks following tracheostomy. It is reported that massive hemorrhage occurring three days to six weeks after tracheostomy is TIF until proven otherwise. Vascular erosion from a tracheostomy tube requires at least 48 hours to develop.5
Diagnosis and Pertinent Anatomy
The innominate artery is the first branch off of the aortic arch. It divides into the right common carotid artery and the right subclavian artery behind the right sternoclavicular joint. The innominate artery runs anterior to the trachea, at approximately the 6th-10th rings, and usually traverses the trachea at the 9th ring.6 A high-lying innominate artery may therefore be a risk factor in formation of TIF. This is also a consideration in controlling bleeding around a tracheostomy site with direct compression.
The condition develops as a connection between the posterior wall of the brachiocephalic trunk and the anterior aspect of the adjacent trachea. On angiography of the brachiocephalic trunk, there may be a small dot of contrast medium accumulation, or no detectable leakage. Bronchoscopy may show no sign of TIF.7,8 The significance of this is clear: bronchoscopy or angiography may not suffice to make the diagnosis in the emergency setting.
Diagnosis of TIF may have to be made on clinical grounds—sudden arterial bleeding from a tracheotomy or ET tube—perhaps with radiographic finding of innominate artery compression by the trachea and/or computed tomography (CT) angiography of the neck and chest. CTA may show no active bleeding source, but may demonstrate that the tip of the tracheal tube is flush with the innominate artery.9 There may be no time in which to perform a CT scan, and as noted above, CTA and laryngoscopy may show no remarkable findings of fistula.10
Clinical Presentation
The patient may present with small amounts of blood from the trachea/ET tube (sentinel bleed), or with frank hemoptysis. There may be pulsatile movements of a tracheal cannula.
 TIF classically develops from three days to six weeks after tracheostomy or insertion of a cuffed endotracheal tube. The clinical manifestation may be either sudden massive tracheal hemorrhage at the tracheostomy site and/or from the endotracheal tube, or a warning/sentinel bleed. Approximately 35-50 percent of patients develop a sentinel bleed prior to life-threatening hemorrhage.11
TIF classically develops from three days to six weeks after tracheostomy or insertion of a cuffed endotracheal tube. The clinical manifestation may be either sudden massive tracheal hemorrhage at the tracheostomy site and/or from the endotracheal tube, or a warning/sentinel bleed. Approximately 35-50 percent of patients develop a sentinel bleed prior to life-threatening hemorrhage.11
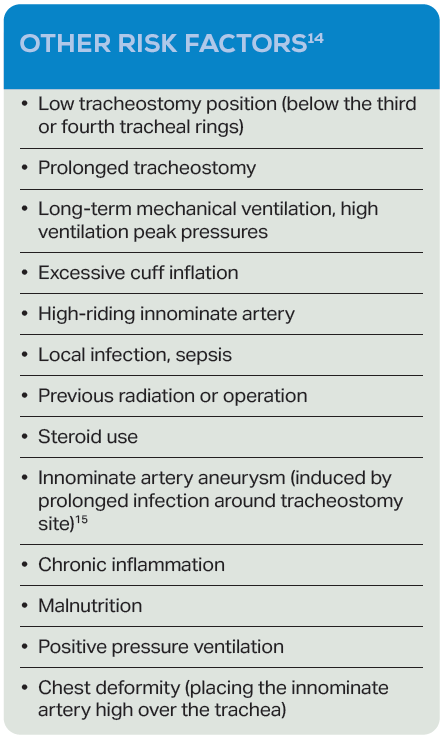
Risk Factors for Development of TIF
High cuff pressures have been implicated, and it is recommended that pressure in a tracheostomy cuff be maintained at less than 20 mm Hg.12 Attention to cuff pressure and tracheal injury appears to stem from the 1970s.13
Emergency Management
The immediate management includes overinflation of the cuff of the tracheostomy or endotracheal tube, and aspiration of blood to clear the airway. The inflation of the tube is done blindly, without any set volume, until the bleeding is stopped. In patients with a tracheostomy in place, use of a tracheostomy cannula with a wired silastic tube has been described to adjust the position of the cuff and using cuff over-inflation to provide hemostasis.4
Maximal inflation of the ETT balloon should be below the level of the tracheostomy. The cuffed tube may be inserted deep into the opening and the cuff expanded, followed by trying the maneuver moving the tube up and re-inflating if the bleeding is not controlled initially. An option if overinflating the tracheostomy cuff does not stop the bleeding is to insert a cuffed oral tracheal tube translaryngeally, then advancing it so that the balloon lies distal to the tracheostomy stoma but above the carina, and withdrawing the tracheostomy tube in order to facilitate simultaneous translaryngeal tracheal intubation. The balloon cuff should be expanded excessively from the lower portion of the bleeding area to prevent accumulation of blood in the lungs.10
If bleeding continues, pressure should be applied to the stoma site. These measures have been reported to control bleeding 80 percent of the time.16 If the patient is hemodynamically stable to undergo bronchoscopy, the major threat to the patient becomes respiratory compromise, so it is recommended to leave the tracheostomy tube in place.5
Manual compression of the innominate artery at the level of the tracheal stoma/manubrium is the Utley maneuver, which applies only for patients who have a tracheal/tracheostomy stoma. Digital compression consists of inserting a finger into the pretracheal space to tamponade the innominate artery against the posterior manubrium or sternum.17 Compression of the innominate artery against the posterior sternum may require enlarging the tracheostoma.18 The finger is inserted through the stoma alongside the endotracheal tube and, while 90 percent success rate has been reported with this method in controlling bleeding, the pressure must be maintained until the patient is transferred to the operating room.10 If a tracheostomy site is present, local compression with a Foley catheter balloon through the tracheostomy site has been described.15
Definitive Treatment
Definitive treatment of TIF has traditionally involved median sternotomy and ligation of the innominate artery. More recently management has involved endovascular stenting of the innominate artery. This may be via a right brachial artery approach to cover the fistula point and avoid the entrance of the common carotid artery.9 Experience with endovascular stenting has been limited, and the rate of endo leak associated with the procedure has been cited as 25 percent, with 50 percent mortality in those requiring bleeding control procedures.15,19 Endovascular intervention depends upon the patient’s hemodynamic stability and availability of interventional radiology.
Bleeding control may involve a right supraclavicular incision/median sternotomy to expose the innominate artery, the right common carotid artery, right subclavian artery and the trachea, and reconstruct the vessel, using vascular clamps to control the bleeding.
Surgery may also entail ligation or resection of the artery with replacement by a vascular prosthesis, carefully maintaining continuity between the right common carotid and the subclavian artery, and placement of a sternocleidomastoid flap, adipose or thymus tissue to cover suture and tracheal defects.20 Reverse saphenous graft has also been employed to produce aorto-carotid and aorto-subclavian anastomoses.21 The tracheal defect may be left adherent to the innominate artery or closed with a pericardial patch.4
Complications
Mortality of TIF has been reported to be above 50 percent, and approaching 100 percent if untreated. Fatal outcomes postoperatively may be due to re-bleeding after attempts to preserve flow in the innominate artery or using sutures or prosthetic material in an infected area.22,23 Ligation of the innominate artery is associated with a risk of brain ischemia and ischemia of the right upper extremity.
The high mortality post-operatively may be related to difficulty in controlling hemorrhage, high infection rates, or other comorbid conditions.24 The fistula is an unclean wound, so that insertion of a stent carries a risk of wound infection. On the other hand, the procedure can be performed under local anesthesia and on an unstable patient. Innominate artery transection also poses a risk of infection such as sternal osteomyelitis after sternotomy—generally required for innominate artery transection—since the surgical field is not aseptic.25
Neurologic deficits have been reported in 10 percent, and sternal wound complications in 39 percent. Many of these patients have preexisting neurologic deficits. Occlusion of the right carotid or right subclavian artery may lead to steal syndrome.26
Conclusion
The incidence of late onset TIF is likely to increase as treatment for patients with severe neuromuscular disorders improves, and these patients’ life expectancy increase. The emergency physician must be prepared to intervene to stabilize these patients and route them to definitve care.
 Dr. Glauser is professor of emergency medicine at Case Western Reserve University at MetroHealth Cleveland Clinic in Cleveland.
Dr. Glauser is professor of emergency medicine at Case Western Reserve University at MetroHealth Cleveland Clinic in Cleveland.
 Dr. Effron is an emergency physician at Metrohealth Medical Center and associate professor of Case Western University in Cleveland.
Dr. Effron is an emergency physician at Metrohealth Medical Center and associate professor of Case Western University in Cleveland.
References
- Cooper JD, Grillo HC. The evolution of tracheal injury due to ventilatory assistance through cuffed tubes: a pathologic study. Ann Surg. 169:334-48.
- Quereshi AZ. Fatal innominate artery hemorrhage in a patient with tetraplegia: case report and literature review. Ann Thorac Cardiovasc Surg. 2013:1960-62.
- Scalise P, Prunk SR, Healy D, et al. The incidence of tracheo-arterial fistula in patients with chronic tracheostomy tubes: a retrospective study of 544 patients in a long-term facility. Chest. 2005;128: 3906-9.
- Furukawa K, Kamohara K, Itoh M, et al. Operative technique for trachea-innominate artery fistula repair. J Vasc Surg. 2014;59:1163-7.
- Grant CA, Dempsey G, Harrison J, et al. Tracheoinnominate artery fistula after percutaneous tracheostomy: three case reports and a clinical review. Br J Anaesth. 2006;96:127-31.
- Oshinsky AE, Rubin JS, Gwozdz GS. The anatomical basis for post tracheostomy innominate artery ruptures. Laryngoscope. 1998;98:1061-64.
- Khanafer A, Hellstern V, Meissner H, et al. Tracheoinnominate fistula: acute bleeding and hemorrhagic shock due to a trachea-innominate artery fistula. CVIR Endovasc. 2021;4(30):1-4.
- Menen RS, Pak JJ, Dowell MA, et al. Treatment of innominate fistula with ligation of the innominate artery: A case report. Perm J. 2016;20:15-6.
- Kakimoto T, Murai S, Kusaka N, et al. A case of trachea-innominate artery fistula after tracheostomy successfully treated with a covered stent. NMC Case Report Journal. 10, 2023;21-5.
- Mun JH, Jun PS, Sim Y-J, et al. Tracheo-innominate artery fistula after stroke. Ann Rehabil Med. 2012;36(6):876-9.
- Taechariyakul T, Keller F, Jahangiri Y. Endovascular treatment of tracheoinnominate artery fistula: case report and literature review with pooled cohort analysis. Semin Thorac Cardiovasc Surg. 2019;32:77-84.
- Kirby RR. The monitoring of mechanically ventilated patients. Int Anesthesiol Clin. 1997;35:65-86.
- Grillo HC, Cooper JD, Geffin B, et al. A low pressure cuff for tracheal tunes to minimize tracheal injury: a comparative clinical trial. J Thorac Cardiovasc Surg. 1971;62:898.
- Dalouee MN, Masoum SHF, Rahnama A, et al. Combined tracheoinnominate artery fistula and tracheoesophageal fistula: A very rare complication of indwelling tracheostomy tube. Lung India. 2016;33(2):225-7.
- Lee SK, Son J-H, Kim YS, et al. Tracheo-innominate fistula caused by isolated innominate artery pseudoaneurysm rupture. J Thorac Dis. 2018;10(7):E577-580.
- Bloss RS, Ward RE. Survival after tracheoinnominate artery fistula. Am J Surg. 1980;139:251-3.
- Utley JR, Singer MM, Roe BB, et al. Definitive management of innominate artery hemorrhage complicating tracheostomy. JAMA. 1972;220:577-9.
- Yun JS, Song SY, Na KJ, et al. Successful surgical management of a trachea-innominate artery fistula in a patient with Duchenne Muscular Dystrophy: a case report. J Chest Surg. 2022;55(1):88-90.
- Ahn HY, Son BS, Kim DH. Recurrent tracheoinnominate artery fistula due to stent graft failure. European J Pediatr Surg Rep. 2015;3:12-14.
- Komatsu T, Sowa T, Fujinaga T, et al. Tracheo-innominate artery fistula: Two case reports and a clinical review. Ann Thorac Cardiovasc Surg. 2013;19:60-2.
- Karunakaran V, Nair NP, Alexander A, et al. Tracheoinnominate artery fistula in a complicated neck penetrating trauma. Turk Arch Otorhinolaryngol. 2020;58(2):127-9.
- Yang FY, Criado E, Schwartz JA, et al. Tracheainnominate artery fistula: retrospective comparison of treatment methods. South Med J. 1988;81:701-6.
- Gelman JJ, Aro M, Weiss SM. Tracheo-innominate artery fistula. J Am Coll Surg. 1994;179:626-634.
- Laswi M, Vega J, Jones K, et al. Tracheoinnominate artery fistula treated with endovascular stent graft at a level I trauma center. Cureus. 12(8):e9710.
- Kaneko S, Uchida K, Karube N, et al. Tracheo-innominate artery fistula with continuous bleeding successfully treated through the suprasternal approach: a case report. J Cardiothorac Surg. 2020;15(1):41.
- Nakai M, Sato H, Sato M, et al. Tracheo-innominate artery fistula successfully treated by endovascular stent-graft repair. Jrn J Radiol. 2013;31:65-70.






No Responses to “How To Manage Tracheo-Innominate Fistula”