
Injuries or soft tissue infections of the lower extremity are common reasons for patients to seek emergency care. Ultrasound-guided regional anesthesia is a key component of multimodal and opioid-sparing pain control in the emergency department.1 Femoral, fascia iliaca, and posterior tibial blocks are lower extremity blocks performed routinely in many emergency departments.2
Explore This Issue
ACEP Now: Vol 39 – No 08 – August 2020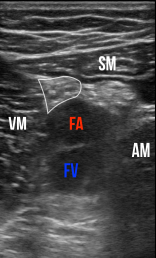
Figure 2: Transverse sonographic view of the adductor canal. The sartorius muscle (SM) forms the “roof.” Vastus medialis (VM) is medial, and the adductor magnus (AM) is lateral. The saphenous nerve (white outline) lies between the femoral artery (FA) and the sartorius. FV is the femoral vein.
images: Peter Croft and David Mackenzie
Blocking the saphenous nerve, often called an adductor canal block, is another valuable tool for emergency clinicians. At the level of the adductor canal, the saphenous nerve is a terminal sensory branch of the femoral nerve. A block provides anesthesia to the medial aspect of the lower leg and ankle as well as the skin overlying a portion of the patella. It is effective for laceration repair or abscess drainage in this distribution and can be used for adjunctive pain relief postoperatively in knee surgeries.3 The adductor canal block is commonly used for analgesia in patients undergoing partial or total knee replacement surgery. Unlike a femoral nerve block, strength in the quadriceps is unaffected, allowing early mobilization or discharge. As with other nerve blocks, ultrasound guidance allows operators to visualize the nerve and can increase the efficacy and safety of the block.1,4
Equipment
Transducer: Select a high-frequency linear transducer (15-6 or 10-5 MHz) with the nerve or soft tissue preset.
Anesthetic: Options include a short- or long-acting anesthetic. Choice depends on the goal of the nerve block: pain relief (preferentially a longer-acting anesthetic) or procedural (preferentially a shorter-acting anesthetic).
- Long-Acting:
- Ropivacaine (max. dose 3 mg/kg), anticipate 6–10 hours analgesia
- Bupivacaine (max. dose 2 mg/kg), anticipate 3–12 hours analgesia
- Short-Acting:
- Lidocaine (max. dose 3 mg/kg), anticipate 1–3 hours analgesia
Research supports using low-dose perineural dexamethasone to prolong the duration of peripheral nerve blocks for several hours.5 A safe choice would be the addition of 2–4 mg of dexamethasone to the volume of anesthetic.
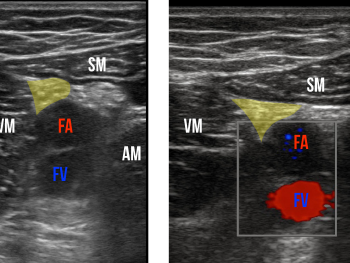
Figure 3: Sonographic view of the adductor canal. The saphenous nerve is highlighted.
Figure 4: Color Doppler flow visualized in the femoral artery and vein. The target saphenous nerve is marked in yellow.
Needle: Choose a 21-gauge or larger needle to optimize visualization. In patients with more soft tissue, a spinal needle may be needed. Consider bringing up a skin wheal of lidocaine to make needle entry less painful. When available, nerve block needles increase echogenicity and may help with visualization, though they are not required to perform an adequate block.
Technique
Pre-Block Assessment: As with any nerve block, assess for distal motor and sensory function along with a distal pulse check.
Patient Positioning: Patient positioning for the adductor canal is relatively easy compared to the ergonomic challenges of some other blocks. Place the patient in a “frog-leg” position (see Figure 1), with the machine on the side of the affected leg and the proceduralist on the opposite side of the bed. (As with any bedside ultrasound procedure, position the machine on the opposite side of the bed from the side of the procedure. This allows a clinician to observe the ultrasound screen comfortably.) While local anesthetic systemic toxicity is rare, cardiac monitoring is technically considered a best practice.1
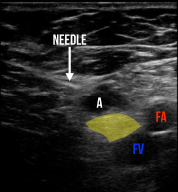
Figure 5: The hyperechoic needle is positioned correctly as the operator administers local anesthetic (A) just above the saphenous nerve (yellow). This in-plane approach provides better visualization of the needle during the procedure.
Ultrasound Landmarks: Position the probe in transverse at the junction between the middle and distal third of the anteromedial thigh. Identify the femoral artery in this area and direct attention to the superomedial aspect of the artery (see Figure 2), which is where the saphenous nerve passes deep to the sartorius muscle. Do not expect the nerve to appear perfectly circular in this region (see Figure 3). Rely on the anatomical consistency that the saphenous nerve will run with the neurovascular bundle of the distal femoral artery and vein in this fascial plane (see Figure 4). Once anesthetic is placed superomedially to the femoral artery and deep to the posterior fascia of the sartorius muscle, the saphenous nerve will become more visible as a result of hydrodissection.
Performing the Block: Using an in-plane approach, direct the needle toward the plane of the vascular bundle while maintaining visualization of the needle tip (see Figure 5). Once the needle pierces through the posterior fascia of the sartorius muscle (you may feel a popping sensation), administer anesthetic. If injected at the correct location, hydrodissection will occur, which, as noted above, often allows for better identification of the nerve. The anesthetic will bathe and envelop the nerve bundle. Avoid injecting directly into the nerve so as to avoid potential nerve injury.
Summary
The adductor canal block is a useful nerve block to facilitate the management of lower extremity soft tissue injuries or infections in the emergency department. It is a valuable addition to other peripheral nerve blocks used commonly by emergency clinicians.
 Dr. Croft is assistant professor of emergency medicine and co-director of the emergency ultrasound division at Maine Medical Center in Portland, Maine.
Dr. Croft is assistant professor of emergency medicine and co-director of the emergency ultrasound division at Maine Medical Center in Portland, Maine.
 Dr. Mackenzie is co-director of emergency ultrasound at Maine Medical Center and assistant professor of emergency medicine at Tufts University School of Medicine in Boston
Dr. Mackenzie is co-director of emergency ultrasound at Maine Medical Center and assistant professor of emergency medicine at Tufts University School of Medicine in Boston
References
- Nagdev A, Dreyfuss A, Martin D, et al. Principles of safety for ultrasound-guided single injection blocks in the emergency department. Am J Emerg Med. 2019;37(6):1160-1164.
- Amini R, Kartchner JZ, Nagdev A, et al. Ultrasound-guided nerve blocks in emergency medicine practice. J Ultrasound Med. 2016;35(4):731-736.
- Vora M, Nicholas T, Kassel C, et al. Adductor canal block for knee surgical procedures: review article. J Clin Anesth. 2016;35:295-303.
- Manickam B, Perlas A, Duggan E, et al. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009;34(6):578-580.
- Pehora C, Pearson AM, Kaushal A, et al. Dexamethasone as an adjuvant to peripheral nerve block. Cochrane Database Syst Rev. 2017;11(11):CD011770.
Pages: 1 2 3 | Multi-Page




No Responses to “How to Perform an Adductor Canal Nerve Block”