The erector spinae plane block (ESPB) is a relatively new block, first described in 2016 as an analgesic technique for neuropathic thoracic pain.1 Since that time, this simple and safe technique has been adopted with enthusiasm and used with great efficacy to treat pain resulting from a wide array of pathological processes. Often referred to as the “poor man’s epidural,” the beauty of this single-injection high-volume block lies in its capacity to anesthetize the majority of the hemithorax. Additionally, the sonoanatomy of the ESPB is relatively simple and safe. Under the erector spinae muscles lie the transverse processes, which act as a bony “backstop” to prevent inadvertent puncture of any critical structures.
Explore This Issue
ACEP Now: Vol 40 – No 09 – September 2021Early uses of the ESPB were for neuropathic chest wall pain, breast surgery, and rib fractures.1–3 Furthermore, the ESPB was found to be particularly efficacious for posterior rib fractures that are typically not amenable to other approaches to thoracic analgesia (ie, the serratus anterior plane block).4 Early case reports have also shown that the ESPB can be applied to lumbar and sacral levels with similar efficacy for abdominal and pelvic pain.5,6 Most notably, some postulate that the ESPB may block sympathetic fibers (in addition to dorsal and ventral rami), thereby relieving visceral pain.7 This would explain a number of studies and case reports that suggest the ESPB may be effective in treating pain associated with visceral thoracoabdominal pathology, including renal colic, pancreatitis, and even appendicitis.8–10 The versatility and simplicity of the ESPB make it a highly useful technique for any emergency physician.
(click to enlarge)
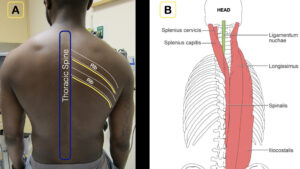
1A) Note the relationship of the thoracic spine, ribs, and intercostal nerves (yellow line).
1B) The erector spinae muscles lie just on top of the spine, forming an ideal target for deposition of anesthetic.
Credit: Arun Nagdev
Anatomy and Innervation
The erector spinae muscles run craniocaudally over the transverse processes, deep in the posterior chest wall (see Figure 1). The ESPB targets this fascial plane and anesthetizes the dorsal rami in addition to the ventral rami and proximal intercostal nerves (see Figure 2). As a result, the ESPB may be able to provide analgesia for the entire hemithorax. The ESPB is a planar block—or more simply, instead of targeting a specific nerve, the goal is to place anesthetic in a defined myofascial plane. Injectate spreads craniocaudally within the fascial plane, permitting analgesia for six to eight rib levels with a single high-volume injection of local anesthetic combined with normal saline flushes (between 20 and 40 mL). The erector spinae fascial plane extends inferiorly into the lumbar and sacral regions as well. Placement location of the ESPB can be adjusted to target the specific spinal levels associated with the painful pathology (eg, injection at T8 is used for pain associated with renal colic).8
(click to enlarge)
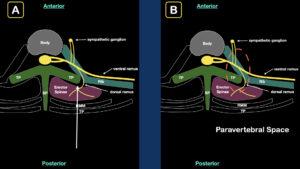
2A) The transverse view of the thoracic spine demonstrates the relationship of the erector spinae muscle, transverse process (TP), and ribs. Note the intercostal spinal nerve as it exits the spinal canal and gives off the ventral ramus, dorsal ramus, and sympathetic ganglion. The white arrow indicates the direction of the injection for an erector spinae plane block.
2B) The goal of the block is to place anesthetic between the erector spinae muscle and the transverse process (TP). Anesthetic is thought to flow into the paravertebral space (orange dashed circle).
Credit: Arun Nagdev
Supplies
- High-frequency linear transducer (13–6 MHz) or low-frequency curvilinear transducer (5–1 MHz), depending on the depth of transverse process.
- Anesthetic: 15–30 mL bupivacaine 0.5% (5 mg/mL; maximum 2 mg/kg). In large-volume plane blocks such as the ESPB, always refer to a reputable weight-based local anesthetic dosing chart.11
- Normal saline flushes 10–20 mL. This can be mixed into the same syringe as the local anesthetic or injected separately to initially open the fascial plane (hydrodissection).
- 100-mm 21-g blunt-tip block needle or 20–22-g Quincke spinal needle. Needle visualization for deep target blocks is significantly easier when using echogenic block needles.
- 91-cm or 36-inch tubing.
- Chlorhexidine skin prep.
- Transparent dressing (Tegaderm) for the transducer and sterile gel packets.
- 25–30-g needle for local skin wheal.
Procedure
- Pre-block
The patient should be placed on continuous cardiac monitoring and pulse oximetry whenever performing a high-volume ultrasound-guided nerve block. Additionally, the clinician should be knowledgeable of the signs, symptoms, and treatment of local anesthetic systemic toxicity (LAST) and have 20% lipid emulsion therapy readily available for this rare but potentially serious complication. (See www.lipidrescue.org for more information.)
- Positioning
The ESPB may be performed with the patient either prone, sitting upright, or in lateral decubitus; the latter we find the most difficult to achieve optimal needle visualization. Needle entry is typically performed cranial to caudal in direction, and the ultrasound machine should be placed in direct line of vision for the operator (see Figure 3 for basic positioning with ultrasound system).

(click to enlarge)
The erector spinae plane block can be performed with the patient supine, upright, or in decubitus.
Credit: Arun Nagdev
- Survey Scan
Level of block: This large-volume planar block will spread craniocaudally, providing multiple levels of analgesia with a single injection. To provide analgesia for rib fractures, choose the spinal level of the middle fracture as a target (eg, T6 for fourth to eighth rib fractures). T7 has been described as an effective target for pain associated with pancreatitis, T8 for renal colic, and L1 for appendicitis.8–10
Start with the probe in longitudinal orientation over the ribs, midway between the scapula and the spine. Note that deep to the ribs, the pleura can be easily identified. Carefully slide the probe medially, looking for the deeper costotransverse junction and then the transverse process (more superficial, wider, and rectangular). If the transducer is placed too medial (past the transverse process), the more deeply located lamina will come into view. The clinician should also note the erector spinae muscle that sits directly over the transverse process. Scan again, back and forth, to differentiate between the deeper (laterally located) rounded ribs with underlying pleura and the targeted, more superficial, and rectangular transverse process, a view in which the pleura is often not visualized (see Figures 4 and 5).
(click to enlarge)
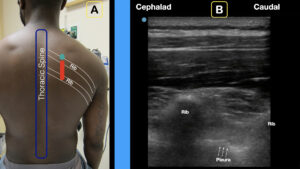
4A) The longitudinal transducer (with probe marker facing cephalad) is placed between the spine and scapula.
4B) Note the ribs (with shadow) and pleura.
Credit: Arun Nagdev
(click to enlarge)
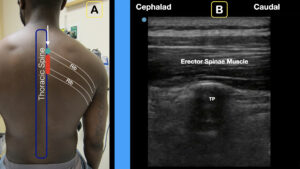
5A) Slide the probe medial until the transverse process is clearly visualized.
5B) The rectangular transverse process (TP) is noted. The erector spinae muscle will sit just superficial to the TP.
Credit: Arun Nagdev
- Skin Wheal
After satisfactory identification of the transverse process (and the overlying erector spinae muscle), widely prep the skin with chlorhexidine, allow it to dry completely, and place a 2–3-mL lidocaine skin wheal 2–3 cm cephalad to the transducer.
- Needle Entry
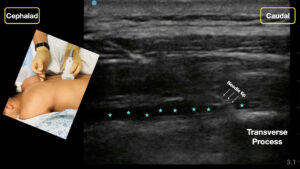
Using an in-plane approach, advance the block needle at a 30º to 45º angle through the trapezius and rhomboid (for blocks at T7 or higher) and then through the erector spinae muscle until the needle tip reaches the posterior surface of the transverse process. After aspiration to ensure no vascular puncture, small aliquots of normal saline are injected to hydrodissect the fascial plane that separates the erector spinae muscle and the transverse process. In our experience, targeting the needle tip at the edge or corner of the rectangular transverse process allows the injectate to hydrodissect the fascial plane more easily. Ensure that the injected anechoic fluid is not placed in the erector spinae muscle but rather is deposited along the fascial plane (see Figure 6, opening of the fascial plane with needle in view). Once satisfied with needle placement, slowly inject the remainder of the 20–40 mL of local anesthetic into the already-open fascial plane.
(click to enlarge)
An in-plane cephalad to caudal approach with clear needle tip is recommended. Note the needle tip and anechoic anesthetic tracks in the fascial plane (green stars).
Credit: Arun Nagdev
Summary
The erector spinae plane block is a simple, safe block that can be applied to a wide variety of painful thoracoabdominal conditions. It is unique in its ability to target both visceral and parietal pain and can be a valuable tool for multimodal pain control in the acute setting. Like with other fascial plane blocks, the clinician should be comfortable using high volumes of injectate, hydrodissecting fascial planes, and recognizing that analgesic onset can be delayed.
Special thanks to Marcus Williams, MD, and Aravind Addepalli, MD, at Highland Hospital for serving as models for the photographs in this article.
References
- Forero M, Adhikary SD, Lopez H, et al. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621-627.
- Gürkan Y, Aksu C, Kuş A, et al. Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: a randomized controlled trial. J Clin Anesth. 2020;59:84-88.
- Riley B, Malla U, Snels N, et al. Erector spinae blocks for the management of rib fractures: a pilot matched study. J Clin Anesth. 2020;63:109780.
- Luftig J, Mantuani D, Herring AA, et al. Successful emergency pain control for posterior rib fractures with ultrasound-guided erector spinae plane block. Am J Emerg Med. 2018;36(8):1391-1396.
- Tulgar S, Aydin ME, Ahiskalioglu A, et al. Anesthetic techniques: focus on lumbar erector spinae plane block. Local Reg Anesth. 2020;13:121-133.
- Kilicaslan A, Aydin A, Kekec AF, et al. Sacral erector spinae plane block provides effective postoperative analgesia for pelvic and sacral fracture surgery. J Clin Anesth. 2020;61:109674.
- Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med. 2017;42(3):372-376.
- Aydin ME, Tekin E, Ahiskalioglu EO, et al. Erector spinae plane block vs non-steroidal anti-inflammatory drugs for severe renal colic pain: a pilot clinical feasibility study. Int J Clin Pract. 2021;75(3):e13789.
- Mantuani D, Luftig J, Herring A, et al. A novel technique to reduce reliance on opioids for analgesia from acute appendicitis: the ultrasound-guided erector spinae plane block. Clin Pract Cases Emerg Med. 2019;3(3):248-251.
- What med? Highland Ultrasound website. Available at: http://highlandultrasound.com/med-guide. Accessed Aug. 13, 2021.
Dr. Mantuani is ultrasound fellowship director at Highland Hospital in Oakland, California. Dr. Yang and Dr. Schultz are ultrasound fellows at Highland Hospital. Dr. Nagdev is director of the ultrasound division at Highland Hospital.
Pages: 1 2 3 4 | Multi-Page





No Responses to “How to Perform an Erector Spinae Plane Block”