
The clavicle is one of the most commonly fractured bones in the human body. Every year, approximately 332,000 people in the United States suffer from a clavicular fracture.1,2 In the emergency department (ED), the focus of treatment is pain control and immobilization unless there is a clear indication for surgery, such as open fractures, skin tenting, or neurovascular compromise.1,2 The mainstay of pain control in the ED has been either oral or intravenous non-steroidal anti-inflammatory drugs (NSAIDs) or opioids.2 However, in our experience these agents commonly do not offer optimal pain control in the acute setting, leading to repeat dosing and, often, prolonged ED stays.
Explore This Issue
ACEP Now: Vol 43 – No 02 – February 2024The ultrasound-guided clavipectoral plane block (CPB) is a newly described technique in the emergency medicine literature.3 The CPB is a simplified technique that can be easily integrated into clinical care by visualizing the deposition of anesthetic in the fascial plane around the clavicle.3,4 While the CPB was first described in the perioperative setting, it may be even more impactful in the ED setting after an acute injury.4-6
1. Anatomy
The clavicle is enwrapped by the clavipectoral fascia, which extends inferiorly from the clavicle, deep to the pectoralis major and superficial to the subclavius muscles. The innervation of the clavicle is poorly understood partly due to anatomical variations.7 The CPB circumvents this issue by directly blocking the terminal sensory nerve endings that innervate the clavicle.3
2. Ultrasound Survey Scan
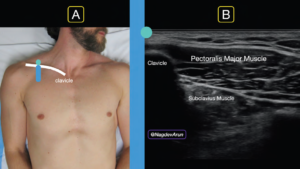
FIGURE 1A: Ultrasound probe should be placed at the clavicle with the probe marker facing cephalad (toward the head).
FIGURE 1B: Ultrasound image with labeled relevant anatomy. (Click to enlarge.)
The clinician should note the fracture site (either via palpable landmark or ultrasound visualization). The initial survey scan should be either just lateral or medial to this site.
The anatomy for the CPB is visualized by placing a linear transducer in a cranial-caudal direction at the midclavicular line with the probe marker towards the patient’s head (Figure 1A). In this position, the pectoralis major and subclavius muscle are located just below the clavicle (Figure 1A). The goal of this simple block is to place anesthetic gently under the fascial plane that defines the border of the pectoralis muscle and the clavicle (Figure 2A, 2B). In our experience, placing anesthetic near the top of the clavicle will separate this potential space and allow for optimal fracture analgesia.

FIGURE 2A: Ultrasound probe placed in a sagittal plane with the probe marker cephalad, in-plane needle technique.
FIGURE 2B: The goal is to visualize the needle tip until it touches the clavicle (red line). (Click to enlarge.)
Once the relevant anatomy is located, place a small skin wheal (2 to 3 ccs of anesthetic) at the inferior aspect of the transducer. Along with marking the entry point for the block, this will provide analgesic for the block.
3. Supplies and Anesthetic
The CPB block uses similar equipment as other ultrasound guided nerve blocks:
- An ultrasound system with a high-frequency 15-6 MHz or 10-5 MHz linear transducer on musculoskeletal or soft-tissue setting
- A blunt-tipped needle: preferably a 20- or 21-gauge regional-block needle
- Appropriately sized syringe to draw local anesthetic; we recommend 20 mL
- 10 mL sterile saline flushes for hydrodissection
- Transparent adhesive ultrasound probe cover (Tegaderm or similar)
- Antiseptic (e.g., alcohol, povidone-iodine, chlorhexidine)
- Sterile ultrasound gel. If available, we recommend using ropivacaine (a concentration of 0.25 percent or less) as it has a longer half-life and a better safety profile than bupivacaine. Weight-based dosing should always be used to prevent local anesthetic systemic toxicity.
4. Performing Procedure

FIGURE 3: The ultrasound system screen needs to be in clear line of sight so that the clinician can see both needle and ultrasound
image. (Click to enlarge.)
Before performing the block, make sure the patient has consented, has intravenous access and is placed on a cardiac monitor.
The patient should be in a supine position. The ultrasound system should be placed so that the operator is able to visualize the point of needle entry, as well as the ultrasound screen in the same line of sight. We commonly place the ultrasound system contralateral to the clavicle that will be blocked (based on what is comfortable for the physician) (Figure 3).

FIGURE 4A: In-plane needle entry.
FIGURE 4B: Needle tip visualized clearly with anesthetic deposited under the clavipectoral fascia. (Click to enlarge.)
Using an in-plane needle approach, enter the skin wheal with a block needle. Visualize the needle tip advancing through the pectoralis major to the inferior aspect of the clavicle (Figure 4A). Ensure continuous needle visualization until the block needle meets the clavicle; resistance may be felt as it goes through the clavipectoral fascia and touches the ostium of the clavicle. We recommend placing the needle at the 12 to 2 o’clock position of the clavicle (Figure 4B). Gently inject 1 to 2 cc of anesthetic to hydrodissect the clavipectoral fascia from the clavicle. The goal is to use the anechoic anesthetic to lift the pectoralis muscle away from the clavicle. This can be visualized with real-time ultrasound guidance. Once the clinician opens this potential space, gently place 3- to 5-cc aliquots, aspirating in between to ensure lack of inadvertent vascular puncture.
Optional
For simplicity and efficiency we recommend a multimodal pain strategy with a single injection site (either medial or lateral to the fracture site) and oral or intravenous medications. Clinicians who have additional time to perform the block can divide the anesthetic dosing and inject medial or lateral to the fracture site.8
For all ultrasound-guided nerve blocks, we recommend placing documentation both in the EHR and as a small skin marking with a surgical pen on the patient. The cardiac monitor should be left on the patient for 30 minutes after the block to assess for local anesthetic systemic toxicity.
Conclusion
Clavicular fractures are common injuries in the ED. The CPB offers a novel technique that can be part of a multimodal pathway along with other agents (NSAIDs, acetaminophen, opioids, etc.) for the ED clinician. Our technique allows a rapid and simplified technique that can provide optimal pain control for patients with clavicle fractures.
Special thanks to our model Justin Bosley, MD.
Dr. Ashworth is a resident physician at Highland Hospital Alameda Health System in Oakland, Calif.
Dr. Lind is an attending physician at Highland Hospital Alameda Health System in Oakland, Calif.
Dr. Martin is director of the emergency ultrasound fellowship at Highland Hospital Alameda Health System in Oakland, Calif.
Dr. Nagdev is director for the emergency ultrasound division at Highland Hospital Alameda Health System in Oakland, Calif.
References
- Postacchini F, Gumina S, De Santis P, et al. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452-456.
- Kihlström C, Möller M, Lönn K, et al. Clavicle fractures: epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord. 2017;18:82.
- Ashworth H, Martin D, Nagdev A, et al. Clavipectoral plane block performed in the emergency department for analgesia after clavicular fractures: A case series. Am J Emerg Med. 2023:S0735-6757(23)00539-9.
- Kukreja P, Davis CJ, MacBeth L, et al. Ultrasound-guided clavipectoral fascial plane block for surgery involving the clavicle: A case series. Cureus. 2020;12:e9072.
- Atalay YO, Mursel E, Ciftci B, et al. Clavipectoral fascia plane block for analgesia after clavicle surgery. Rev Esp Anestesiol Reanim (Engl Ed). 2019;66(10):562–563.
- Abu Sabaa MA, Elbadry AA, El Malla DA: Ultrasound-guided clavipectoral block for postoperative analgesia of clavicular surgery: A prospective randomized trial. Anesth Pain Med. 2022;12:e121267.
- Tran DQ, Tiyaprasertkul W, González AP: Analgesia for clavicular fracture and surgery: A call for evidence. Reg Anesth Pain Med. 2013;38:539-543.
- Lee CCM, Beh ZY, Lua CB, et al. Regional anesthetic and analgesic techniques for clavicle fractures and clavicle surgeries: Part 1-A scoping review. Healthcare (Basel). 2022;10:1487.
Pages: 1 2 3 4 | Multi-Page





One Response to “How To Perform an Ultrasound-Guided Clavipectoral Block”
February 28, 2024
Doc_CWhy not simply a superficial cervical plexus block more on the caudal side to get the rami claviculares of the cervical plexus?
Cheers