Over the past few years, emergency physicians have begun implementing multimodal strategies for acute pain, reducing the use of opioids. Ultrasound-guided single-injection nerve blocks have slowly become accepted for targeted pain relief over the past decade in the emergency department for hip fractures, rib fractures, deltoid abscess drainage, and other conditions.1–3 Currently, point-of-care ultrasound (POCUS) fellowships require ultrasound-guided nerve blocks as part of the training curriculum to ensure future leaders will provide the next generation of emergency physicians the knowledge to offer optimal pain management.4,5
Explore This Issue
ACEP Now: Vol 38 – No 05 – May 2019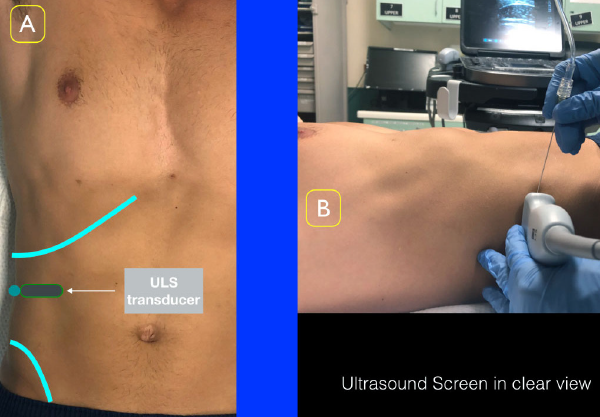
Figure 2A: Place the ultrasound transducer between the inferior costal margin and iliac crest. The probe marker should point lateral/posterior. Figure 2B: Position the ultrasound screen to ensure clear view of the location of injection as well as the ultrasound screen.
Over the past decade, our group has been fortunate to work in a hospital that values interdepartmental collaboration to optimize patient care. More often than not, long delays for patients admitted for surgical pathology (such as acute appendicitis) lead to repeated rounds of intravenous opioid analgesics that ultimately fail to achieve adequate pain control and feature side effects. This led our group to think of alternative methods for pain control in this population rather than standard intravenous opioid regimens.
The ultrasound-guided transversus abdominis plane (TAP) block is a well-established regional anesthetic block used by anesthesiologists for perioperative pain control of the anterior abdominal wall.6,7 At our center, after computed tomography (CT) confirmation of appendicitis, ED-performed TAP blocks have been instituted as an alternative analgesic option for alleviating pain from this common diagnosis. This additive analgesic (in addition to other intravenous agents) has proved effective in our small cohort of patients, who have demonstrated reduced pain scores and need for additional pain medications while awaiting definitive surgical intervention.8
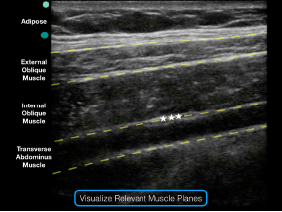
Figure 3: Note the external oblique, internal oblique, and transverse abdominis muscles on the ultrasound screen. The goal is to deposit anesthetic in the potential space just above the transverse abdominis muscle and just below the internal oblique muscle.
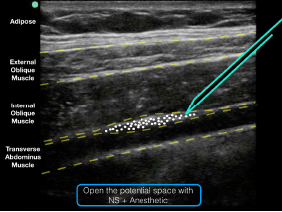
Figure 5: An ultrasound representation demonstrating where anesthetic should be placed when performing a TAP block.
The Procedure
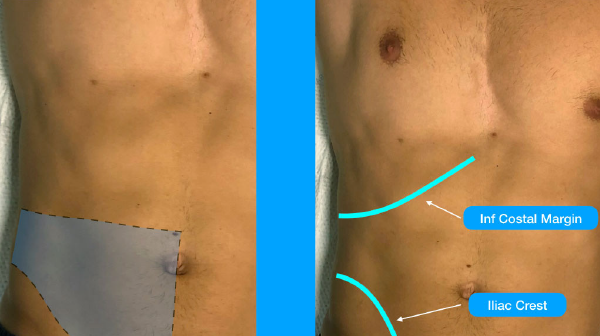
After consent, place your patient supine and exposed from the inferior costal margin to the iliac crest, the two surface landmarks for the procedure (see Figures 1A and 1B). Place a high-frequency (13–6 MHz) linear array transducer in transverse orientation above the iliac crest at the mid- to anterior-axillary line (see Figures 2A and 2B) so that the external oblique, internal oblique, and transversus abdominis muscle layers are easily visualized on ultrasound (see Figure 3). This allows for optimal access to your target point: the plane between the internal oblique and transversus abdominis muscles.
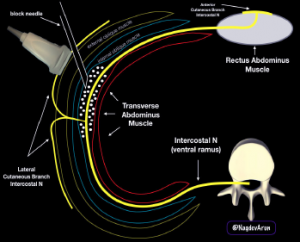
Figure 4: A schematic drawing of the ultrasound-guided TAP block. Note that anesthetic fluid should track in the plane between the internal oblique and transverse abdominis muscles.
Place the ultrasound system in a location contralateral to the patient for a clear view of the block field and the ultrasound screen. For convention, we place the transducer directional marker to the patient’s right. Inject a 1–2 mL anesthetic wheal adjacent to the transducer (the needle will enter medially and go lateral/posterior). When optimal visualization is achieved, place a 20- to 22-guage 90-mm blunt-tipped block needle in-plane (medial to lateral/posterior) and advance it until the needle reaches the interfascial plane between the internal oblique and transverse abdominis muscles. Using a two-person hand-on-needle technique, inject between 20 mL and 30 mL of a long-acting local anesthetic, which are the weight-based dosing limits of bupivacaine and lidocaine with epinephrine (see Figures 4 and 5). Successful deposition can be confirmed on ultrasound by visualization of anechoic fluid tracking in between the internal oblique and transverse abdominis muscles.
Conclusion
Acute pain management is the responsibility of the emergency physician. Multimodal pathways that allow clinicians a method to tailor pain management to the needs of the patient will reduce the reliance on opioid-only algorithms and improve patient care. Our multidisciplinary model for treating pain from acute appendicitis has proved successful due to a non-siloed approach to offering best practices to our patients.
References
- Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20(6):584-591.
- Durant E, Dixon B, Luftig J, et al. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2017;35(1):197.e3-197.e6.
- Herring AA. Bringing ultrasound-guided regional anesthesia to emergency medicine. AEM Educ Train. 2017;1(2):165-168.
- Lewiss RE, Tayal VS, Hoffmann B, et al. The core content of clinical ultrasonography fellowship training. Acad Emerg Med. 2014;21(4):456-461.
- Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound: consensus recommendations from the 2008 Council of Emergency Medicine Residency Directors Conference. Acad Emerg Med. 2009;16(4):S32-36.
- Niraj G, Searle A, Mathews M, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103(4):601-605.
- Tsai HC, Yoshida T, Chuang TY, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:8284363.
- Mahmoud S, Miraflor E, Martin D, et al. Ultrasound-guided transverse abdominis plane block for ED appendicitis pain control. Am J Emerg Med. 2019;37(4):740-743.
Pages: 1 2 | Multi-Page





No Responses to “How To Perform an Ultrasound-Guided TAP Block for Appendicitis Pain”