
Bedside transthoracic echocardiography (TTE) has become an invaluable tool in emergency and critical care medicine. Bedside assessment of the presence or absence of a pericardial effusion, gross ejection fraction, size of the right ventricle, and cardiac activity during cardiopulmonary resuscitations has become standard in residency training and general practice.1
Explore This Issue
ACEP Now: Vol 39 – No 07 – July 2020In the past few years, a growing group of emergency department sonographers has
pioneered work in how transesophageal echocardiography (TEE) performed at the bedside may provide similar utility. Like the previous generation of clinicians who were able to teach legions of ED sonographers to perform various exams at the bedside, these sonographers have helped the availability of TEE at the bedside start to become a reality.
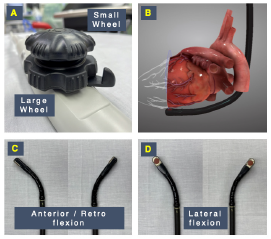
Figure 2: Mechanical controls of a TEE probe. (A) A large wheel controls anteflexion, as required to obtain a transgastric short axis view (B) and retroflexion (C). A small wheel performs lateral flexion (D).
TEE offers a few clear advantages over the classic TTE performed in most emergency departments today. First, because the probe visualizes the heart through the esophagus, the windows are excellent and easy to obtain (the lungs, ribs, and habitus do not interfere). Second, TEE allows the sonographer to be off the chest during active CPR, facilitating visualization of the heart continuously to guide management while not interrupting compressions. TTE can be used for assessing fluid responsiveness in mechanically ventilated patients, the guidance of pacemaker placement, and the guidance of extracorporeal membrane oxygenation (ECMO) cannulation during initiation of extracorporeal circulation (ECPR).
Given its reliability in providing high-quality images regardless of patient-related or external factors that often limit TTE, TEE represents a powerful tool for the delivery of critical care.2–4
Once a modality used only for comprehensive examinations, over the last two decades TEE has expanded from its traditional diagnostic indications (ie, cardiac surgery, suspected endocarditis, or cardioversion in atrial fibrillation) to assist the evaluation and management of patients with acute hemodynamic decompensation, shock, and cardiac arrest in operative and nonoperative environments.
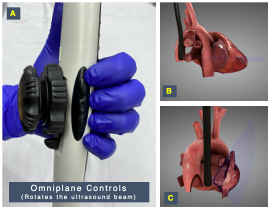
Figure 3: (A) Lateral buttons allow for digital rotation of the ultrasound beam (omniplane) generated in the probe head. (B) Rotation between 0° and 180° using these buttons allows the probe to develop views in multiple planes such as coronal or transverse (note the purple omniplane axis). (C) The four-chamber view or sagittal plane in a bicaval view is shown for comparison.
3-D graphics reproduced with permission by HeartWorks Intelligent Ultrasound
The use of TEE in the emergency department and critical care settings, often defined as “focused” or “resuscitative” to describe its goal-directed nature and differentiate the scope and objectives of application from comprehensive or consultative TEE, has been shown to be feasible, safe, and clinically impactful in the emergency and intensive care settings, and its use has been supported by society guidelines.1–4
In this article, we aim to provide a practical overview on the use of resuscitative TEE for emergency physicians.
Why Do We Need Resuscitative TEE in the ED?
Echocardiography represents a valuable component in the evaluation of unstable patients, including those with undifferentiated shock and in cardiac arrest. In many settings, TTE guides resuscitations during the critical phase of care, can determine rapidly reversible causes, and can identify when efforts may be futile. Unfortunately, optimal views can be a challenge; recent data show that integrating TTE into cardiac arrests may inadvertently prolong compression pause duration.5 Some of the common factors limiting the quality of TTE images include body habitus and emphysema.
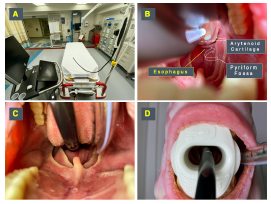
Figure 4: Probe insertion technique. (A) The TEE probe handle should be hung or held by an assistant to allow free movement of the shaft. (B) The probe should be inserted maintaining midline to avoid common sites of obstruction at the arytenoid cartilages and pyriform fossae. (C) Once at the base of the tongue at midline, a “chin lift” maneuver will facilitate passage by opening the esophagus. (D) Once in place, a bite block previously loaded into the probe should be placed to avoid damage by the teeth on the probe.
Felipe Teran
In our experience, we have found three primary applications where TEE can prove useful and influential in the emergency department.
- Guiding Cardiac Arrest Resuscitation: The primary indication for use of resuscitative TEE in the emergency department is during cardiac arrest.3,4 In addition to the same diagnostic and prognostic qualities provided by TTE images, including the identification of reversible causes such as cardiac tamponade or pulmonary embolism (PE), TEE also provides advantages during resuscitation. Recent animal and human data have shown that standard cardiac compressions may not squeeze the left ventricle but rather the left ventricular outflow tract. TEE allows rapid adjustment of the compression location and may result in higher rates of return of spontaneous circulation (ROSC).6 Also, chest compression interruptions can be limited because the probe can obtain optimal views of the heart during active CPR.7
- Evaluation and Management of Shock in Intubated Patients: Although TTE remains the first-line modality for the assessment of patients in shock in the emergency department, TEE is a powerful alternative for intubated patients in whom TTE windows are inadequate or unavailable. Once placed, TEE can help establish the etiology or predominant mechanism of shock, perform serial hemodynamic assessments estimating stroke volume (SV) and SV variation, determine preload sensitivity using respirophasic variation of superior vena cava diameter, and monitor hemodynamic interventions (ie, initiating or titrating vasopressor therapy).8–10
- Procedural Guidance: In addition to its diagnostic value and usefulness as a hemodynamic monitoring tool, resuscitative TEE has a unique role guiding several emergency procedures, such as initiation and monitoring ECMO, and the placement of intravenous pacemaker wires.11,12
TEE Safety
The risks associated with comprehensive TEE examinations have been studied extensively in the perioperative and echocardiography laboratory environments. Major complications such as oropharyngeal trauma, esophageal perforation, and major bleeding are exceedingly rare, with incidence rates ranging between 0.01 and 0.08 percent.13–16 Furthermore, in the resuscitative setting, the risk of these complications is often outweighed by the benefit of obtaining time-sensitive and lifesaving information, making the safety profile of TEE comparable to many other commonly performed emergency procedures.
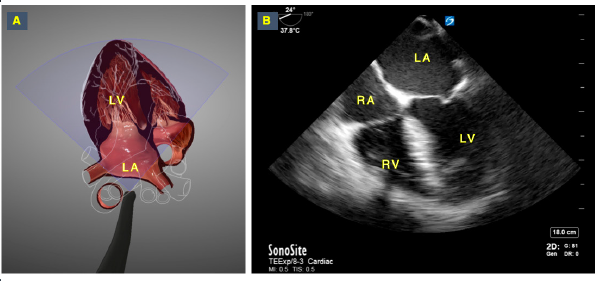
Figure 5: Retrocardiac “point of view” of the TEE probe. Image A shows the TEE probe’s point of view, which provides sonographers with an ideal perspective to understand the spatial orientation and anatomical relationships needed to develop and interpret TEE views. Image B shows the corresponding mid-esophageal 4 chamber view in TEE, with the left atrium in the near field.
3-D graphics reproduced with permission by HeartWorks Intelligent Ultrasound
How to Perform Resuscitative TEE
TEE Probe Knobology: In place of the normal hand movements used when performing TTE (eg, fanning, sliding, rotating, etc.), the TEE probe uses mechanical digital components to produce the desired images. The endoscopic shaft may be advanced, withdrawn, and turned to locate the heart. The lockable wheels on the handle then help produce the various movements similar to tilting, fanning, and rocking the probe by anteflexing and retroflexing the transducer (see Figures 1 and 2).
In addition to these mechanical controls, digital components allow for rotation of the imaging plane itself (the ultrasound beam) in a 180° plane. This is referred to as the omniplane, and it’s displayed by a half circle with a range of 0–180° located at one of the top corners of the screen. The utilization of the omniplane allows for further characterization and detailed views of the heart and surrounding structures. This movement is similar to looking at structures in the long and short axis when utilizing a TEE probe (see Figure 3).
Probe Insertion: Resuscitative TEE is generally performed only in intubated patients. The placement of the TEE probe is performed similarly to the placement of an orogastric tube. The flexion wheels are first placed in the unlocked position to allow for free movement of the probe tip. With the transducer facing anteriorly, the probe is advanced into the mouth and pharynx under direct vision and manual guidance to maintain midline position.
The most common anatomical sites causing obstruction of the TEE probe during insertion in an intubated patient are the arytenoid cartilage and the pyriform fossa. Therefore, to access the esophagus and avoid pharyngeal injuries, it is critical to keep the probe at the midline while advancing it. This can be performed by either digitally guiding the probe or under direct visualization with a video laryngoscope.
To aid in the passage of the probe tip past the upper esophageal sphincter, the mandible may be pulled forward gently and the patient’s neck partially flexed. Be careful not to dislodge the endotracheal tube (see Figure 4).
Acquiring and Interpreting TEE Images: Understanding the anatomical position of the heart is fundamental to the practice of echocardiography and particularly for TEE. A new mental representation of the cardiac anatomy is required to comprehend how images are generated from the esophageal position when performing TEE. This is the view most anatomy textbooks and echocardiography learning resources use to display the heart, and it is the view that makes the most sense to understand how TTE views are generated.
On the other hand, to interpret TEE views, a different anatomical perspective must be understood. The TEE probe head is located in the esophagus and obtains images from a retrocardiac perspective. This inverted imaging position is often difficult for even seasoned TTE sonographers, but it is the starting point in understanding TEE imaging. Simply put, this new perspective is the view of the heart and great vessels as seen by the TEE probe when the image is generated from the esophageal position. This retrocardiac perspective facilitates the understanding of how the different mechanical and digital movements in TEE generate the views obtained while using this modality (see Figure 5).
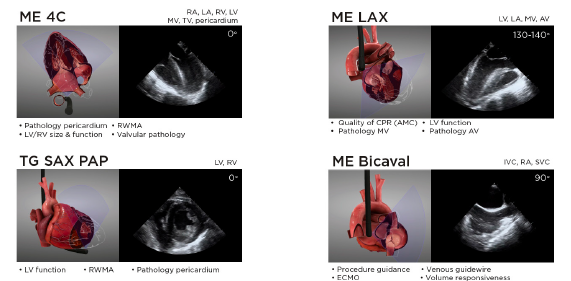
Figure 6: Summary of the views and main clinical applications of the four core resuscitative TEE views. Additional views can be used on a case-by-case basis to answer questions and guide management in specific clinical scenarios. Some of these views include mid-esophageal 2C (ME 2C), mid-esophageal aortic valve and ascending aorta short and long axis (ME AV SAX, ME ascending aorta SAX/LAX), right ventricular inflow-outflow (ME RV I-O), descending thoracic aorta (DTA SAX and LAX), and deep transgastric 5 chamber (Deep TG 5C). A full protocol including additional resuscitative TEE views can be found at www.resuscitativetee.com/protocols.
The right atrium (RA) and right ventricle (RV) are relatively anterior cardiac structures. Meanwhile, the left atrium (LA) and left ventricle (LV) are posterior structures. The LA is the closest structure to the esophagus at the mid-esophageal level, so the ultrasound beam passes through this structure first. This is why mid-esophageal views have the LA located in the near field of the image and can be conceived as the scanning window to visualize the heart in TEE. The heart lies anterior and slightly left in relation to the esophagus, with the LA “leaning” against the esophagus. The right heart is situated anteriorly within the mediastinum and is the farthest structure from the esophagus, which is why, unlike in TTE, in TEE the RV is seen in the far field of the image.
Imaging Planes and Resuscitative TEE Views
Four core TEE views are most commonly used in resuscitative settings and provide the highest yield of information. These include mid-esophageal 4 chamber (ME 4C), mid-esophageal long axis (ME LAX), transgastric short axis at the level of papillary muscles (TG SAX PAP), and mid-esophageal bicaval (ME bicaval).
Developing the cognitive and motor skills needed to acquire and interpret these views proficiently, like any other imaging modality, takes practice. In our experience, simulation training is essential in both skill acquisition and maintenance of competency. Therefore, we recommend that clinicians who would like to incorporate TEE into their clinical care find a resuscitative TEE hands-on course to provide them with structured training, then supplement that training with mentored training in live patients (see Figure 6).
Conclusion
Emergency medicine has rapidly developed from its early days into a dynamic field in which experts push boundaries in optimal clinical care. Resuscitative TEE is yet another attempt to both define our growing specialty while offering the best care for our critically ill patients. Acute care physicians (including emergency medicine) will continue to define indications of TEE and to expand the field, integrating this novel technology into our scope of practice.
Today, it has become standard for many ED clinicians to perform bedside transthoracic ultrasound in the evaluation of a hypotensive or dyspneic patient. In the near future, TEE will become another invaluable tool during the resuscitation in the emergency department.
As William Gibson once said, “The future is here. It’s just not evenly distributed yet.”
Dr. O’Neil is chief resident in the department of emergency medicine at the Hospital of the University of Pennsylvania in Philadelphia.
Dr. Nagdev is director of emergency ultrasound at Highland General Hospital, Alameda Health System in Oakland, California.
Dr. Teran is clinical instructor of emergency medicine in the division of emergency ultrasound and Center for Resuscitation Science, Department of Emergency Medicine, at the University of Pennsylvania.
References
- Teran F. Resuscitative cardiopulmonary ultrasound and transesophageal echocardiography in the emergency department. Emerg Med Clin North Am. 2019;37(3):409-430.
- Arntfield R, Pace J, Hewak M, et al. Focused transesophageal echocardiography by emergency physicians is feasible and clinically influential: observational results from a novel ultrasound program. J Emerg Med. 2016;50(2):286-294.
- Teran F, Dean AJ, Centeno C, et al. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140-147.
- Fair J, Mallin M, Mallemat H, et al. Transesophageal echocardiography: guidelines for point-of-care applications in cardiac arrest resuscitation. Ann Emerg Med. 2018;71(2):201-207.
- Clattenburg EJ, Wroe P, Brown S, et al. Point-of-care ultrasound use in patients with cardiac arrest is associated prolonged cardiopulmonary resuscitation pauses: a prospective cohort study. Resuscitation. 2018;122:65-68.
- Catena E, Ottolina D, Fossali T, et al. Association between left ventricular outflow tract opening and successful resuscitation after cardiac arrest. Resuscitation. 2019;138:8-14.
- Fair J 3rd, Mallin MP, Adler A, et al. Transesophageal echocardiography during cardiopulmonary resuscitation is associated with shorter compression pauses compared with transthoracic echocardiography. Ann Emerg Med. 2019;73(6):610-616.
- Vignon P, Mentec H, Terré S, et al. Diagnostic accuracy and therapeutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest. 1994;106(6):1829-1834.
- Mayo PH, Narasimhan M, Koenig S. Critical Care Transesophageal Echocardiography. Chest. 2015;148(5):1323-1332.
- Vieillard-Baron A, Chergui K, Rabiller A, et al. Superior vena caval collapsibility as a gauge of volume status in ventilated septic patients. Intensive Care Med. 2004;30(9):1734-1739.
- Fair J, Tonna J, Ockerse P, et al. Emergency physician-performed transesophageal echocardiography for extracorporeal life support vascular cannula placement. Am J Emerg Med. 2016;34(8):1637-1639.
- Lerner RP, Haaland A, Lin J. Temporary transvenous pacer placement under transesophageal echocardiogram guidance in the emergency department. Am J Emerg Med. 2019;S0735-6757(19)30834-4.
- Hilberath JN, Oakes DA, Shernan SK, et al. Safety of transesophageal echocardiography. J Am Soc Echocardiogr. 2010;23(11):1115-1221.
- Daniel WG, Erbel R, Kasper W, et al. Safety of transesophageal echocardiography. A multicenter survey of 10,419 examinations. Circulation. 1991;83(3):817-821.
- Kallmeyer IJ, Collard CD, Fox JA, et al. The safety of intraoperative transesophageal echocardiography: a case series of 7,200 cardiac surgical patients. Anesth Analg. 2001;92(5):1126-1130.
- Ramalingam G, Choi SW, Agarwal S, et al. Complications related to peri-operative transoesophageal echocardiography – a one-year prospective national audit by the Association of Cardiothoracic Anaesthesia and Critical Care. Anaesthesia. 2020;75(1):21-26.





No Responses to “How to Perform Resuscitative Transesophageal Echocardiography in the Emergency Department”