The ultrasound-guided distal sciatic nerve block is the ideal block for patients with distal leg and ankle injuries (large lateral leg laceration, pain reduction from bimalleolar fractures, Achilles tendon rupture, lower leg burns, abscesses, etc.). Depending on the anesthetic used, the block can facilitate fracture reduction or abscess drainage or be used as an adjunct in a multimodal plan for pain control. Unfortunately, the superficial structures of the medial lower leg and ankle are not innervated by the distal sciatic nerve, and a saphenous nerve block (distal aspect of the femoral nerve) may be needed if a more complete analgesia to the lower leg is desired.
Explore This Issue
ACEP Now: Vol 34 – No 06 – June 2015The block can facilitate fracture reduction or abscess drainage or be used as an adjunct in a multimodal plan for pain control.
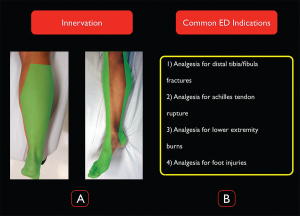
Indications
The distal sciatic nerve innervates the majority of the lower extremity below the knee, making it an ideal block for ankle and distal tibial/fibular fractures and injuries to the foot (see Figure 1). It does not provide anesthesia to the medial aspect of the lower leg, which is innervated by the saphenous nerve (a distal branch of the femoral nerve).
(Click for larger image)
Figure 1. Distal sciatic nerve innervation and common ED indications for the block. Credit: Arun Nagdev
Contraindications
Any injury that could potentially result in compartment syndrome is a relative contraindication to performing a distal sciatic nerve block. High-energy injuries such as a solitary tibial or mid-shaft tibial/fibular fracture are known to have high rates of developing compartment syndrome. Additionally, crush injuries or any injury with associated vascular
(Click for larger image)
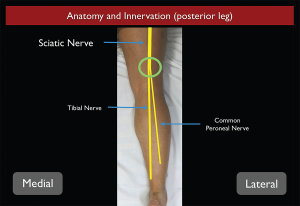
Figure 2. Sciatic nerve anatomy from the posterior aspect as it travels down the thigh into the leg. Credit: Arun Nagdev
compromise should trigger a detailed discussion with consultative services (orthopedics, trauma surgery, etc.) before an ultrasound-guided distal sciatic nerve block in the popliteal fossa is performed.
Anatomy
The distal sciatic nerve originates from the L4-S3 nerve roots of the lumbar-sacral plexus. The sciatic nerve initially runs deep in the posterior thigh, gradually becoming more superficial as it approaches the popliteal fossa. The large sciatic nerve bifurcates into the tibial (medial) and the common peroneal (lateral) nerves approximately 7–10 cm proximal to the popliteal fossa (see Figure 2). At this level, the sciatic nerve is bound by the semimembranosus and semitendinosus muscles medially and the biceps femoris muscle laterally. Although the sciatic nerve can be blocked at any location along its course, its superficial position in the region of the popliteal fossa makes this distal location ideal.1,2
Patient Positioning
If possible, the patient should be in the prone position, allowing easy access to the popliteal fossa and posterior aspect of the patient’s lower extremity. In a patient who is unable to lie prone (cervical spine immobilization, etc.), the affected extremity must be elevated and supported with mild flexion of the knee. This is best achieved by propping the foot with blankets or pillows to allow the ultrasound probe to easily fit between the popliteal fossa and the patient’s bed. Either position will allow the clinician to block the sciatic nerve in the popliteal fossa, with the prone position being technically much less difficult.
Equipment/Probe Selection
A high-frequency linear probe should be used to image the distal sciatic nerve in the popliteal fossa (see Figure 3). We recommend a 20- or 22-gauge, 3.5-inch (9 cm) spinal needle to reach the distal sciatic nerve because of its depth in the popliteal fossa. In addition, 20 mL of local anesthetic will be needed.
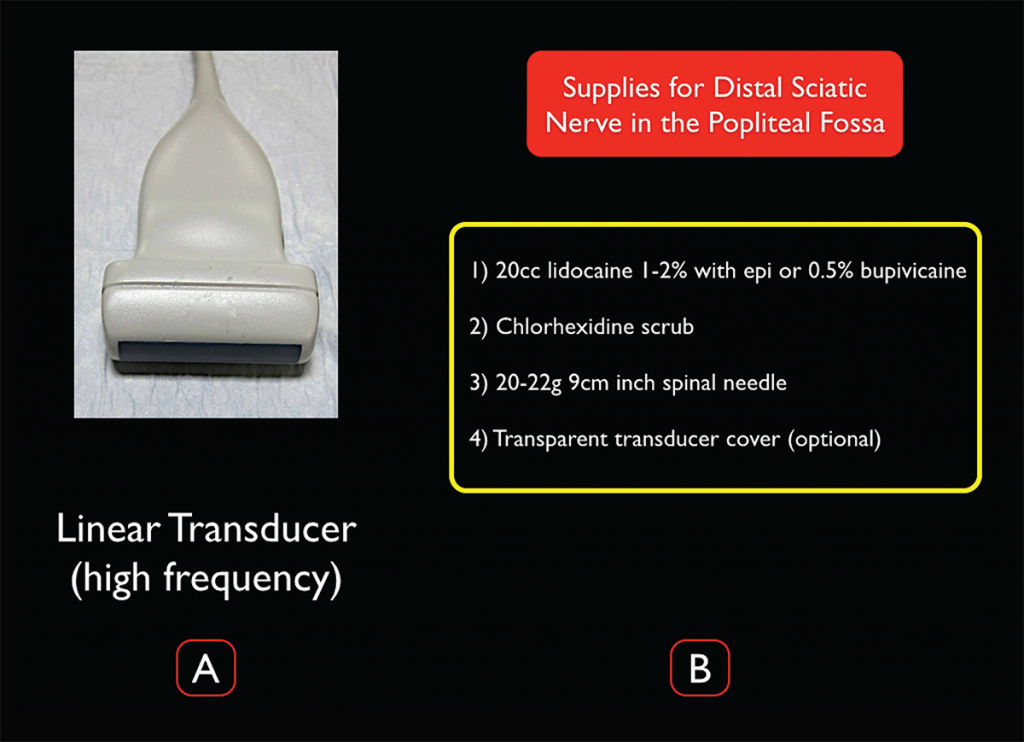
(Click for larger image)
Figure 3. Transducer and supplies needed for ultrasound-guided distal sciatic nerve block in the popliteal fossa. Credit: Arun Nagdev
Survey Scan
To prepare for the block, start by placing the high-frequency linear probe with the probe marker facing the patient’s right side at the popliteal crease and identify the popliteal artery and vein. The tibial nerve is commonly located just superficial to the popliteal vein and appears as a hyperechoic honeycomb-like structure (see Figure 4). If you are unable to locate the neural bundle, fan the probe caudal to cephalad to obtain the most perpendicular axis to the nerve, which allows for better visualization (an ultrasound phenomenon termed anisotropy). Once the tibial nerve is visualized, follow the nerve proximally until it joins with the common peroneal nerve (lateral) to form the distal sciatic nerve (see Figure 5). The operator should mark this location and note the depth of the nerve and distance from the lateral thigh to ensure the appropriate length of needle prior to starting the procedure.
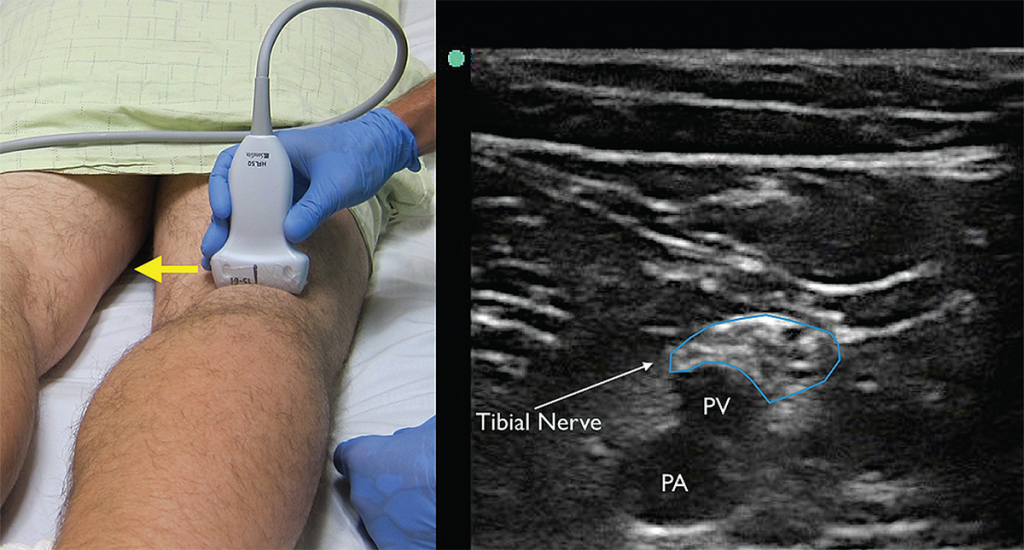
(Click for larger image)
Figure 4. The tibial nerve sits just above the popliteal artery (PA) and popliteal vein (PV). Identification of this nerve is the first step in identifying the larger and more proximal distal sciatic nerve. Yellow arrow indicates direction of probe marker. Credit: Arun Nagdev
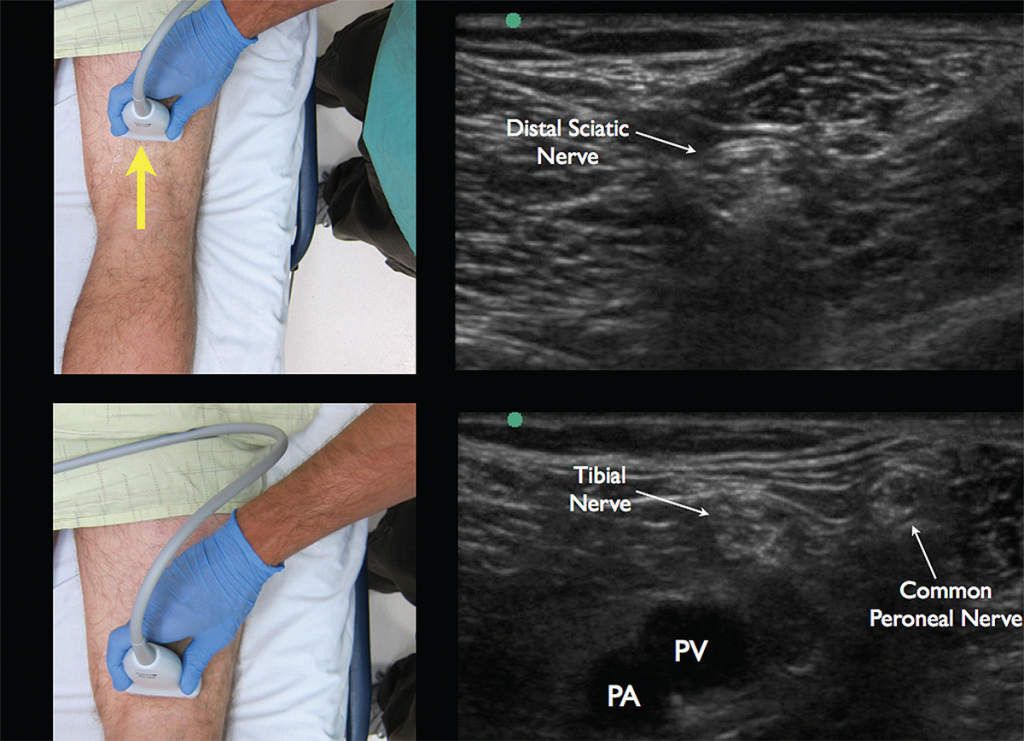
(Click for larger image)
Figure 5. Appropriate movement of the ultrasound probe cephalad to visualize the joining of the tibial nerve with the common peroneal nerve forming the distal sciatic nerve. Note the common peroneal nerve approaching from the lateral aspect. Credit: Arun Nagdev
Procedure
The distal sciatic nerve is often 2–4 cm under the skin surface, making for a steep needle angle if entering the skin just adjacent to the ultrasound transducer (like most other ultrasound-guided nerve blocks). Instead, we recommend measuring the depth of the nerve during the initial survey scan and entering the lateral leg with a flat angle to ensure clear needle visualization. After placing a small skin wheal (on the lateral aspect of the thigh), fill 20 mL of local anesthetic in a syringe attached to a 20–22 gauge, 3.5-inch (9 cm) spinal needle. The more lateral approach and depth of the distal sciatic nerve often necessitate the longer needle for an in-plane distal sciatic nerve block.
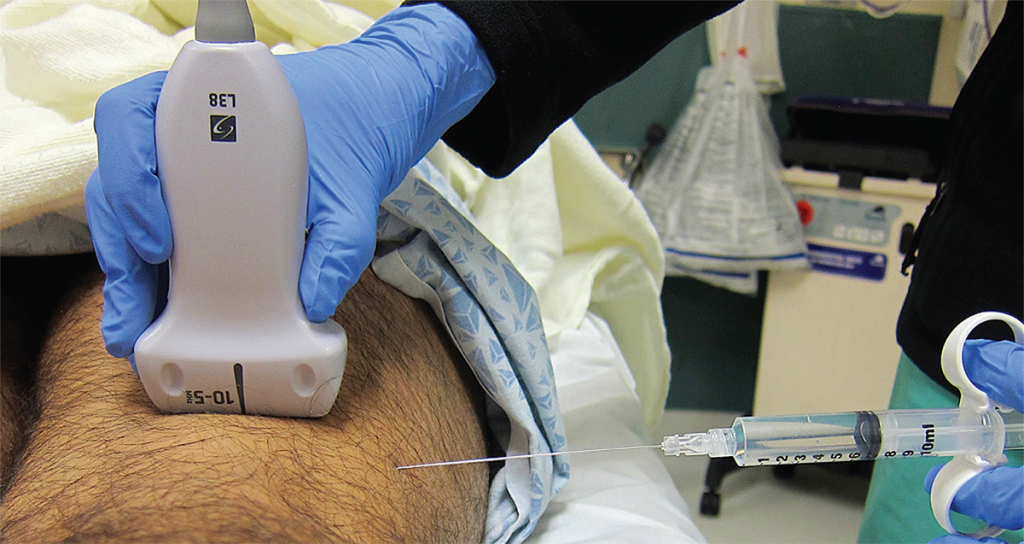
(Click for larger image)
Figure 6. Ultrasound and needle placement for the distal sciatic nerve block in the popliteal fossa. Note the flat needle entry lateral to the transducer. Credit: Arun Nagdev
Even though some experienced users may prefer the out-of-plane technique, we feel that the in-plane lateral to medial approach is both easier and safer for the novice sonographer. Slowly advance the spinal needle maintaining a nearly parallel angle to the probe with an in-plane technique (see Figure 6). Since the needle will be entering the lateral thigh, the needle tip will not be visualized immediately (like in other in-plane blocks), and the operator will often have to advance the needle a few centimeters until the tip will be seen entering the scanning plane. Attempt to place the needle tip on the superficial edge of the distal sciatic nerve without penetrating the nerve bundle (see Figure 7A). It is often difficult to determine whether the needle tip is either in the superficial tissue or the fascial plane of the nerve. Injecting small aliquots of either anesthetic or normal saline and visualizing its
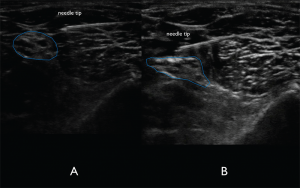
(Click for larger image)
Figure 7A. In-plane lateral to medial approach of the needle. The needle tip is visualized clearly to ensure lack of nerve and vasculature puncture.Figure 7B. Spread of anechoic local anesthetic surrounding the distal sciatic nerve indicating a successful nerve block. Credit: Arun Nagdev
spread can be the discriminatory test to ensure that the needle tip is in the correct location. Once in the correct location, aspirate to confirm lack of vascular puncture, then slowly inject 2–3 mL aliquots of anesthetic until spread of anechoic fluid is noted to track around the distal sciatic nerve (see Figure 7B). Fanning the probe proximally and distally without moving the needle can be a simple method to confirm tracking of fluid in the fascial plane. We do not recommend novice sonographers place the needle tip on the inferior aspect of the nerve given its relative proximity to the popliteal vasculature. The sciatic nerve in the popliteal fossa has a significant complex fascial sheath. If there is difficulty visualizing anesthetic tracking along the nerve, the operator may need to place the needle tip through the complex fascial sheath, which can resemble epineurium. Often, the operator will feel a “pop” when puncturing the fascia. Using normal saline or very small aliquots of anesthetic under ultrasound visualization will then show a clear demarcation of nerve and fascia.3,4
Complications
Intravascular injection should be a concern because of the proximity of the popliteal vasculature and the distal sciatic nerve. A flat needle angle will allow for clear needle tip visualization and hopefully reduce chances of either local anesthetic systemic toxicity or peripheral nerve injury.
References
- Marhofer P, Harrop-Griffiths W, Willschke H, et al. Fifteen years of ultrasound guidance in regional anaesthesia: part 2—recent developments in block techniques. Br J Anaesth. 2010;104:673-683.
- Murray JM, Derbyshire S, Shields MO. Lower limb blocks. Anaesthesia. 2010;65:57-66.
- Herring AA, Stone MB, Fischer J, et al. Ultrasound-guided distal popliteal sciatic nerve block for ED anesthesia. Am J Emerg Med. 2011;29:e3-5.
- Tirado A, Nagdev A, Henningsen C, et al. Ultrasound-guided procedures in the emergency department-needle guidance and localization. Emerg Med Clin North Am. 2013;31:87-115.
Dr. Johnson and Dr. Lovallo are in the department of emergency medicine at Alameda Health System’s Highland Hospital in Oakland California.
Dr. Mantuani is an attending physician in the department of emergency medicine and director of internal medicine point-of-care ultrasound at Highland Hospital.
Dr. Nagdev is director of emergency ultrasound at Highland Hospital in Oakland, California, and assistant clinical professor (volunteer) of emergency medicine at the University of California, San Francisco.
Pages: 1 2 3 4 | Multi-Page




No Responses to “How to Perform Ultrasound-Guided Distal Sciatic Nerve Block in the Popliteal Fossa”