Running an effective and evidence-based cardiac arrest resuscitation is a core skill for all emergency physicians. To identify reversible causes of pulseless electrical activity (PEA), emergency physicians have integrated point-of-care ultrasound (POCUS) into care for this group of critically ill patients. Specifically, during the brief 10-second pause of cardiopulmonary resuscitation (CPR), the goal is to rapidly assess for signs of cardiac tamponade, massive pulmonary embolism or other reversible causes of arrest. Unfortunately, two emergency medicine studies have demonstrated that emergency department POCUS use during the resuscitation of out-of-hospital cardiac arrests may inadvertently prolong CPR pauses, which has been shown to negatively impact survival.1,2 Multiple regression analysis demonstrated that POCUS was associated with longer pauses (6.4 s, 95%CI 2.1- 10).8 We believe that with some minor adjustments, we can effectively and safely incorporate POCUS into cardiac arrest resuscitation. Additionally, a recent novel concept from the resuscitation literature allows the clinician to take advantage of the benefits of imaging, while ensuring high-quality uninterrupted CPR.
Explore This Issue
ACEP Now: Vol 42 – No 09 – September 2023Simple Steps to Improve Quality CPR When Using POCUS
The resuscitation of the patient in cardiac arrest can be difficult for even the most seasoned clinician. Protocolization of POCUS can offer a reduction in cognitive burden during this demanding period. Data at our institution and another large academic emergency department indicated that physicians were inadvertently increasing the duration of CPR pauses when using POCUS, forcing us to develop a simplified clinical POCUS pathway. ACEP Now’s three-step cardiac arrest sonographic assessment (CASA) protocol asked the clinician to rapidly (in under 10 sec) answer one question during each CPR pause.3
Look for a pericardial effusion on the first pause, right ventricular (RV) strain on the second pause, and cardiac activity on the third pause. Each step was meant to streamline the CPR pause duration, while also allowing the clinician to determine the need to act on a reversible cause of the cardiac arrest. During active compressions, the clinician could also examine the thoracic cavity for the presence of a large pneumothorax, and the abdomen for the presence of intra-abdominal fluid.
As expected, integration of this simplified protocol over the past five years has resulted in a decrease in CPR pause duration at our institution. We also have implemented simple adjuncts (in addition to the CASA protocol) to ensure high-quality CPR.
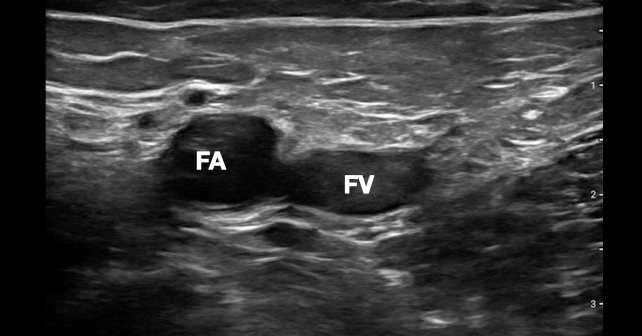
- Find the echo view before pause: During CPR, the clinician who is performing POCUS should attempt to find the ideal view of the heart. Often, this is a subxiphoid view, but can also be a parasternal long or apical four-chamber view (see Figure 1). The goal is to have a reasonable view before the CPR pause so that time is not wasted finding an adequate window.4

FIGURE 1: A) Subxiphoid view demonstrating a pericardial effusion with signs of echocardiographic tamponade B) Apical four-chamber (A4C) view demonstrating right ventricular strain in a patient with a massive pulmonary embolism C) Three views of the heart when attempting to find a good window to image during cardiac compressions. (Click to enlarge.)
- Use a 10-second clock: Our nurse recorder for the code counts out loud from 10 to one during the pause so that the scanning clinician knows when to get off the chest. Chest compressions are always started at the end of the 10 seconds unless return of spontaneous circulation(ROSC) or a shockable rhythm is recognized. Also, we have set our recording timer on our ultrasound systems to six seconds so that the clinician is aware of the duration of the recording.
- Review clip during CPR: The clinician records the ultrasound clip during the pause and then interprets the video after CPR restarts.
- Stay off the chest after showing there is no pericardial effusion or signs of right ventricle (RV) strain: Each time the probe is placed on the chest for evaluation of cardiac activity, the physician risks a prolonged pause. Once POCUS has ruled out potential reversible causes of cardiac arrest (tamponade or RV strain), avoid excessive, repeat, cardiac ultrasound evaluations during CPR pauses. The goal at this point is to identify ROSC.
Modification to the CASA Protocol
After the first two steps of the CASA exam are negative (there is no clinically significant pericardial effusion or RV strain), our standard technique was to identify the presence of cardiac activity (at each subsequent pause), as a surrogate marker for ROSC. Unfortunately, there is significant variability between physicians when assessing for the presence of cardiac activity.5 Additionally, there is uncertainty as to what degree of cardiac activity generates sufficient perfusion to safely stop CPR. From our clinical experience, there have been many instances when slight but concentric cardiac activity is noted on POCUS without a palpable pulse, making it unclear if CPR should continue. Recent data using ultrasound evaluation of the femoral artery have helped change the way we employ ultrasound in cardiac resuscitation. Instead of using our phased array transducer to assess for the presence or absence of cardiac activity (with the worry of prolonging CPR pause time and misinterpreting the presence of enough cardiac activity to produce a perfusable blood pressure),we have moved to the femoral region for imaging during CPR pauses. We switch to a linear probe, and image the femoral artery using B-mode as a surrogate for ROSC.
Switching to a linear probe and imaging at the common femoral artery has become our third step in our cardiac arrest ultrasound algorithm because this approach is faster and more reliable than subjectively feeling for a pulse. Ultrasound is more than twice as sensitive for the presence of a pulse than manual palpation.6 Using a linear probe to identify pulsatility of the femoral or carotid artery has been shown to be more accurate than manual palpation for pulses, and can almost always be done in less than five seconds.6 This modification removes the clinical sonographer from the chest, decreasing prolonged pauses in CPR. The simplest way to look for a pulse with ultrasound is to place a linear probe on the inguinal crease and identify the common femoral artery during ongoing compressions. The right femoral region is commonly selected because the first two steps of the CASA protocol are usually performed from the right side of the patient. The goal is to apply enough pressure to collapse the femoral vein, and look for pulsatility of the femoral artery (see Figure 2).
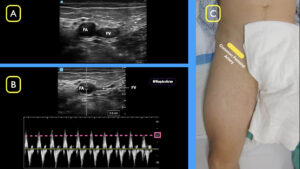
FIGURE 2: A) Compress the common femoral vein (FV) and visualize pulses in the common femoral artery (FA) B) Using spectral doppler, define a peak systolic velocity (PSV) >20 cm/sec C) Using a linear probe in the inguinal crease, locate the common femoral artery and vein. (Click to enlarge.)
In addition to using B-mode ultrasound to determine the presence or absence of a femoral pulse during a cardiac resuscitation, spectral or gated Doppler can be added at the same location to identify whether there is a perfusable rhythm. Work by Gaspari, et al., defined that some patients previously thought to have PEA are now recognized as having “pseudo-PEA,” where the heart is beating in an organized manner but a pulse cannot be manually palpated due to low cardiac output.7 This scenario raises the question of how to identify if sufficient cardiac perfusion is present that CPR is no longer needed. Recent studies show that applying gated Doppler to the femoral artery can identify patients who have achieved ROSC whether or not they have a palpable pulse.8 In practical terms, if femoral arterial pulsation is present on B-mode ultrasound during a pulse check, the next step is to use the spectral Doppler function to measure the peak systolic velocity, which may be used to define a perfusable pressure (or ROSC). This technique allows the clinician to determine the presence of a perfusable rhythm and may be even more sensitive than a rise in the end-tidal CO2, which was previously considered the first sign of ROSC.9
Technique
Place the linear probe at the inguinal crease and look for pulsation of the common femoral artery on B-mode. Additionally, prior to the CPR pause, press the Doppler button and move the Doppler gate over the femoral artery. When the CPR pause starts, press the Doppler button again to measure a Doppler waveform. Keeping your non-scanning hand over the Doppler button as the CPR pause approaches will minimize delay to waveform recording. Freeze the waveform image and measure the maximum amplitude of the peak systolic velocity. A value of greater than 20 cm/sec has been shown in some studies to correlate to a systolic blood pressure over 60 mmHg (see Figure 2).9
Conclusion
Incorporating POCUS into the resuscitation of a patient in cardiac arrest is an important skill for the emergency physician. A protocolized algorithm and simple techniques to reduce CPR pauses allows POCUS to be integrated without the inadvertent complication of prolonging CPR pauses. Bedside imaging allows clinicians to diagnose reversible causes rapidly as well as to define endpoints for resuscitation. We use the initial steps of the CASA protocol to ensure that there are no acutely reversible causes on the first two CPR pauses, but then move to the right femoral region with a linear transducer once these steps are complete. Along with defining the presence of pulses with higher accuracy, we employ femoral artery Doppler waveform to determine the presence of a perfusable rhythm. This adjustment to our resuscitation protocol is one way to stay off the chest during compressions while also employing POCUS to help improve the care of our sickest patients.
Dr. Martin is director of resident and medical student ultrasound education at Highland Hospital/Alameda Hospital in Oakland, Calif.
Dr. Howell is an ultrasound fellow at Highland Hospital/Alameda Health System in Oakland, Calif.
Dr. Nagdev is director of emergency ultrasound at Highland Hospital/Alameda Health System in Oakland, Calif.
Dr. Desai is an ultrasound fellow at Highland Hospital/Alameda Health System in Oakland, Calif.
References
- Clattenburg EJ, Wroe PC, Gardner K, et al. Point-of-care ultrasound use in patients with cardiac arrest is associated prolonged cardiopulmonary resuscitation pauses: A prospective cohort study. Resuscitation. 2018;122:65-68.
- Huis In ’t Veld MA, Allison MG, Bostick DS, et al. Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation. 2017;119:95-98.
- Clattenburg EJ, Wroe PC, Gardner K, et al. Implementation of the cardiac arrest sonographic assessment (CASA) protocol for patients with cardiac arrest is associated with shorter CPR pulse checks. Resuscitation. 2018;131:69-73.
- Gaspari R, Harvey J, DiCroce C, et al. Echocardiographic pre-pause imaging and identifying the acoustic window during CPR reduces CPR pause time during ACLS – A prospective cohort study. Resusc Plus. 2021;6:100094.
- Hu K, Gupta N, Teran F, et al. Variability in interpretation of cardiac standstill among physician sonographers. Ann Emerg Med. 2018;71(2):193-198.
- Kang SY, Jo IJ, Lee G, et al. Point-of-care ultrasound compression of the carotid artery for pulse determination in cardiopulmonary resuscitation. Resuscitation. 2022;179:206-213.
- Gaspari R, Weekes A, Adhikari S, et al. A retrospective study of pulseless electrical activity, bedside ultrasound identifies interventions during resuscitation associated with improved survival to hospital admission. A REASON Study. Resuscitation. 2017;120:103-107.
- Cohen AL, Li T, Becker LB, et al. Femoral artery Doppler ultrasound is more accurate than manual palpation for pulse detection in cardiac arrest. Resuscitation. 2022;173:156-165.
- Haddad G, Margius D, Cohen AL, et al. Doppler ultrasound peak systolic velocity versus end tidal carbon dioxide during pulse checks in cardiac arrest. Resuscitation. 2023;183:109695.
Pages: 1 2 3 4 | Multi-Page





No Responses to “How To Safely Incorporate Ultrasound Into Cardiac Arrest Resuscitation”