Airway technology has advanced rapidly in recent years and many emergency departments (EDs) now stock video laryngoscopes with hot-swappable disposable blades, second-generation laryngeal masks that are easier to place and designed to transmit an endotracheal tube, and single-use flexible endoscopes that bring the capabilities of conventional fiber-optic bronchoscopes to emergency settings. These advances introduce novel airway management options that are not yet widely utilized.1 One particularly powerful example is the use of a flexible endoscope to facilitate tube delivery after the larynx has been exposed using a video laryngoscope. We call this video-assisted flexible endoscopic intubation VAFEI, pronounced “vaffy.”
Explore This Issue
ACEP Now: Vol 41 – No 11 – November 2022The VAFEI Procedure
Preparation
- Preoxygenate and hemodynamically optimize the patient as time and physiology allow.
- If fully awake approach is undertaken, patient should be pretreated with antisialagogue and diligent topicalization of local anesthesia.
- Equipment list:
- Intubating flexible endoscope (FE) preloaded with endotracheal tube
- Video laryngoscope (VL) blade (hyperangulated geometry particularly advantageous but standard-geometry blade also effective)
- Topical anesthetics (e.g., four percent lidocaine via atomizer) if non-paralyzed approach
- Usual intubation and difficult airway equipment (e.g., suction, capnography, supraglottic device, cricothyrotomy materials)
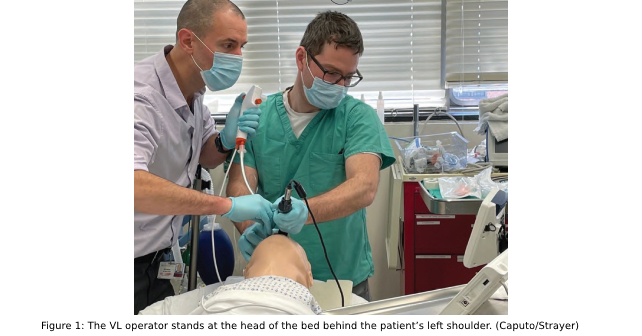
- Positioning (Figure 1):
- VL operator stands at the head of the bed behind the patient’s left shoulder.
- FE operator stands at the head of the bed behind the patient’s head.
- Patient should be positioned in semifowler position.
- Screens (single split-screen is ideal) positioned over the patient’s bed in front of operators.
Airway Pharmacology
- If rapid sequence intubation (RSI) is undertaken, simultaneously administer sedative and paralytic agent.
- If non-paralyzed ketamine-only approach is undertaken, administer dissociative dose or titrated sub-dissociative doses of ketamine until patient is adequately induced.
- Application of atomized lidocaine to the larynx blunts cough and gag reflexes and reduces the chance of vocal cord spasm during ketamine-only approaches.
- When induced, VL operator performs laryngoscopy as usual to obtain adequate view (or, if difficult anatomy prevents adequate view, obtain best possible view). The VL operator, maintaining laryngoscope position with left hand, readies suction in right hand, in preparation for flexible endoscopy.
- Once VL operator obtains their view, the FE operator looks into the mouth, places the scope in the patient’s mouth, and advances to the end of the blade under direct visualization. The FE operator looks at the VL screen to guide the FE to the vocal cords.
- If performing an awake/breathing intubation, vocal cords may be anesthetized with four percent lidocaine via the utility port on the bronchoscope or using a mucosal atomization device.
- The FE operator then advances the FE through the cords, either under guidance of the VL screen or, if VL screen view is inadequate, using the FE screen (see Video 1 and Video 2 on our website).
- The FE operator advances the scope beyond the vocal cords until the carina is visualized.
- The FE operator or assistant railroads the preloaded endotracheal tube (ETT) beyond the vocal cords until the tip is seen on the FE screen.
- The FE operator withdraws the scope, visualizing the tip of the ETT just proximal to the carina to confirm proper positioning.
- The ETT is then attached to a bag valve mask (BVM) or ventilator circuit with waveform capnography to confirm gas exchange.
Pearls and Pitfalls
VAFEI is a simple procedure that can become complex if rushed. The right speed is slower than one’s instincts. Use suction liberally. If the airway is soiled, the VL operator must assertively suction fluids.
Preload the endotracheal tube with the tube’s natural curvature in the conventional orientation, with the bevel facing to the left.
Contemporary VL and FE scopes are heated to reduce the likelihood of fogging, but fogging may still occur and is improved by the use of defogging ointment, if available. Alternatively, if fogging of the endoscope occurs, gently press the tip of the scope against the patient’s mucosa to defog. If obstructive anatomy impedes advancing the flexible endoscope, the ETT itself can be used as a conduit; i.e., advance the tube beyond the FE until passage is clear to cords, then advance the scope through the tube and then through the cords. When advancing the tube, if there is a hold-up at the arytenoids, withdraw the tube slightly, then rotate the tube counterclockwise as you advance (left at the larynx, right at the rings for hold-up).2 The VL must be held in place for the entire FE procedure, including as the ETT is railroaded over the scope. Maintaining VL position distracts obstructive tissues and allows visual confirmation of procedural steps.
A convenience sample of 10 patients intubated using the VAFEI technique is described in Table 1.
Discussion
VAFEI has been described in operating room-based literature, including a randomized controlled trial that demonstrated benefit versus usual video laryngoscopy across a series of outcomes.3,4,5 An emergency department-based case report described the technique with a channeled video laryngoscope, but it has received little attention as an intubation strategy in emergency medicine.6 VAFEI takes advantage of the strengths of each modality to address the weaknesses of the other. Though any blade shape can be used, VAFEI is particularly well-suited for use with hyper-angulated VL (HAVL), as steeply curved blades provide an optimal view of the glottis, but intubation failures and delays with HAVL are often attributable to difficulty maneuvering a styletted ETT to the glottis and then through the cords, down the trachea.7-10 The flexible endoscope overcomes tube delivery difficulties commonly encountered during HAVL as the operator “drives” the scope around the primary and secondary airway curves that confound immobile stylets.11
The use of a video laryngoscope facilitates flexible endoscopy and addresses key barriers to the use of FE in emergency settings. Most importantly, the laryngoscope clears a path through the mouth for the endoscope, allowing it to be manually inserted to the glottic inlet. This obviates the need to navigate the nose and nasopharynx, and reduces the difficulty in steering around the tongue and other oral structures. From an operator skills perspective, VAFEI can be likened to a bougie technique rather than a conventional flexible endoscopic intubation technique.
Unlike traditional awake flexible endoscopy, VAFEI can be performed very rapidly, which allows the procedure to be incorporated into an RSI-based paralyzed approach. RSI maximizes the likelihood of first pass success and for decades has been used in the majority of emergency department intubations.12,13,14,15
VAFEI can be used as part of a topically anesthetized awake approach, however achieving sufficient local anesthesia that an awake patient will tolerate laryngoscopy requires more time than is available in many emergency intubation cases and is enabled by specialized equipment (e.g., atomizers, concentrated lidocaine) that may not be available.
VAFEI can also be incorporated into a ketamine-only strategy that attempts to take advantage of the safety benefit of ATI by maintaining spontaneous respirations while overcoming the challenges in executing effective topicalization, by using enough ketamine that the patient will tolerate laryngoscopy and tracheal intubation.16 The use of atomized lidocaine about the posterior oropharynx and glottis is still recommended, if feasible, to attenuate airway reflexes and laryngospasm that may impede tube delivery even in dissociated patients.
The primary drawback of the VAFEI technique is that it requires two operators: one to perform video laryngoscopy and one to advance the flexible endoscope. However, both operators need not be physicians, and in fact one operator can perform VAFEI by first completing laryngoscopy and then handing off the VL to an assistant positioned to the operator’s left, behind the patient. VAFEI requires that both VL and FE devices be available and ready, which is a barrier in many departments; however, the emergence of single-use, disposable VL blades and endoscopes allows wider adoption of this technology in emergency settings. Operation of the flexible endoscope in VAFEI does not require the same degree of skill as is needed to perform conventional flexible endoscopic intubation, but does require familiarity with the device and its basic functions, which can easily be acquired in a simulation training session.
Conclusion
VAFEI is a powerful intubation technique that takes advantage of the strengths of video laryngoscopy and flexible endoscopy while diminishing their drawbacks.17 It can be incorporated into approaches that preserve spontaneous ventilation and performed quickly enough to be used with paralysis and rapid sequence intubation. Because most anatomically difficult airways are unpredicted, it is essential that airway management strategies plan for first-attempt failure.18,19,20
Dr. Strayer is an emergency physician at Maimonides Medical Center, in Brooklyn.
Dr. Caputo is associate chief of the Department of Emergency Medicine at NYC H+H/Lincoln Medical Center in the South Bronx.
References
- Berkow LC, Morey TE, Urdaneta F. The technology of video laryngoscopy. Anesthesia & Analgesia. 2018;126(5):1527-1534.
- Ho AM, Ho AK, Mizubuti GB. Tracheal intubation: The proof is in the bevel. J Emerg Med. 2018;55(6):821-826.
- Lenhardt R, Burkhart MT, Brock GN, Kanchi-Kandadai S, Sharma R, Akça O. Is video laryngoscope-assisted flexible tracheoscope intubation feasible for patients with predicted difficult airway? A prospective, randomized clinical trial. Anesth Analg. 2014;118(6):1259-65.
- Driver BE, Prekker ME, Reardon RF, Fantegrossi A, Walls RM, Brown CA III. Comparing emergency department first-attempt intubation success with standard-geometry and hyperangulated video laryngoscopes. Ann Emerg Med. 2020;76(3):332-338.
- Ahmad IN, Ali NE, Liming BJ. Direct laryngoscopy assisted fiberoptic intubation: A novel technique for the pediatric airway. Int J Pediatr Otorhinolaryngol. 2020;137:110232.
- Sowers N, Kovacs G. Use of a flexible intubating scope in combination with a channeled video laryngoscope for managing a difficult airway in the emergency department. J Emerg Med. 2016;50(2):315-9.
- Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM. Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011 Jan;114(1):34-41.
- Gu Y, Robert J, Kovacs G, et al. A deliberately restricted laryngeal view with the GlideScope® video laryngoscope is associated with faster and easier tracheal intubation when compared with a full glottic view: a randomized clinical trial. Can J Anaesth. 2016;63(8):928-37.
- Kelly FE, Cook TM. Seeing is believing: Getting the best out of video laryngoscopy. Br J Anaesth. 2016;117 Suppl 1:i9-i13. doi: 10.1093/bja/aew052.
- Greenland KB, Edwards MJ, Hutton NJ, Challis VJ, Irwin MG, Sleigh JW. Changes in airway configuration with different head and neck positions using magnetic resonance imaging of normal airways: a new concept with possible clinical applications. Br J Anaesth 2010;105:683-90.
- Levitan R, Heitz J, Sweeney M, Cooper R. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2010;57:240-7.
- Li J, Murphy-Lavoie H, Bugas C, Martinez J, Preston C. Complications of emergency intubation with and without paralysis. Am J Emerg Med. 1999;17(2):141-3. doi: 10.1016/s0735-6757(99)90046-3.
- Bouska R, Sakles J, Stolz U, Mosier J. Rapid sequence intubation compared to sedation only for out-of-or intubations using video laryngoscopy. The Journal of Emergency Medicine. 2014;46(2):279.
- Walls RM, Brown, CA III, Bair AE, Pallin DJ, NEAR III Investigators. Emergency airway management: a multi-center report of 8937 emergency department intubations. J Emerg Med. 2011;41:347-354.
- Brown CA III, Bair AE, Pallin DJ, Walls RM, NEAR III Investigators. Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med. 2015;65:363-370.
- Merelman AH, Perlmutter MC, Strayer RJ. Alternatives to rapid sequence intubation: contemporary airway management with ketamine. west j emerg med. 2019;20(3):466-471.
- Riegel AK, Winterhalter M. Combining videolaryngoscopy with fiber-optic orotracheal intubation for inclusion in the nonemergency pathway of the difficult airway algorithm. A A Pract. 2019;12(1):28-29.
- Nørskov AK, Rosenstock CV, Wetterslev J, Astrup G, Afshari A, Lundstrøm LH. Diagnostic accuracy of anaesthesiologists’ prediction of difficult airway management in daily clinical practice: a cohort study of 188,064 patients registered in the Danish Anaesthesia Database. Anaesthesia. 2015;70(3):272-81. doi:10.1111/anae.12955.
- Hayden E, Pallin D, Wilcox S, et al. Emergency department adult fiberoptic intubations: incidence, indications, and implications for training. Acad Emerg Med. 2018;25(11):1263–7.
- Mazzinari G, Rovira L, Henao L, et al. Effect of dynamic versus stylet-guided intubation on first-attempt success in difficult airways undergoing glidescope laryngoscopy: a randomized controlled trial. Anesth Analg. 2019;128(6):1264-1271.






No Responses to “How To Use Video-Assisted Flexible Endoscopic Intubation”