
Transferring patients from one ED to another hospital is an established part of emergency medicine practice. Patients who need inpatient services do not match the index hospitals’ capabilities, or the patient requests such a transfer, or the hospital has no available inpatient space. The rate of transfers was stable for many years, typically around 2 percent.
Explore This Issue
ACEP Now: Vol 43 – No 06 – June 2024Transfers have always been an area of concern to hospital administrators and emergency physicians. In 1986, Congress enacted the Emergency Medical Treatment and Labor Act (EMTALA) to ensure public access to emergency services regardless of ability to pay. Section 1867 of the Social Security Act imposes specific obligations on Medicare-participating hospitals that offer emergency services to provide a medical screening examination (MSE) when a request is made for examination or treatment for an emergency medical condition (EMC), including active labor, regardless of an individual’s ability to pay. Participating hospitals are then required to provide stabilizing treatment for patients with EMCs. If a hospital is unable to stabilize a patient within its capability, or if the patient requests, an appropriate transfer should be implemented. This law, along with many court rulings since its enactment, makes all patient transfers an area of review and concern.
Two years ago, an ACEP Now article covered the issue of transfer challenges resulting from early pandemic operations.1 As fresh challenges of the pandemic and hospital operations changed emergency medicine practice, one of the more challenging areas was the movement of admitted patients out of the first emergency department (ED). Many EDs have been unable to move admitted patients into appropriate inpatient beds in any hospital, and the result has been inpatients stacked in hallway beds in the ED.
A recent study from JAMA Network Open highlighted the issues of patient transfers, particularly for small rural hospitals.2 Their study was limited to 681 hospitals and characterized transfer patterns related to caseload-constrained hospitals. They reported concerns related to overcoming barriers to transferring patients in future surges.
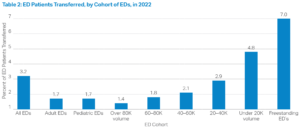
In fact, that study underestimated the ongoing challenges affecting patient transfers in U.S. emergency departments. Transfer rates are up across all types of EDs. In the last couple of years, EDs have transferred 3.2 percent of patients—twice the rate in 2010 (Table 1).
The data additionally show the ongoing transfer rate is higher in small volume EDs (4.7 percent). ED transfer rates vary dramatically by cohorts, increasing by nearly a factor of three for hospital-based EDs with decreasing volume (Table 2).
What Is the Burden of These Patients on EDs and Ambulance Providers?
The ED volumes seen in the U.S. in 2023 will be reported at around 160 million patients. At a 3.2 percent transfer rate, that is about 5.1 million patients being transferred in a year, or almost 14,000 patients a day. That patient movement stresses all types of hospitals and requires consideration of EMTALA requirements with each one. These tallies do not include freestanding EDs, which have an estimated transfer rate of about 7 percent.
This only represents ED transfers. Some hospitals also must transfer patients out of inpatient units when patient needs cannot be managed in the original hospital. This results in a significant caseload for ambulance transport services that provide the bulk of patient movement.
Moving Toward Solutions to Flow of Admitted and Transfer Patients
The management of admitted patients for prolonged periods of time is a current problem for all EDs. The issue of inpatient boarding compromising ED operations has been widely reported.3 The additional lengthy ED stays for transfer patients are equally resource-intense for emergency physicians and especially emergency nurses. Some hospital systems have developed transfer centers or flow centers, which attempt to coordinate patient movement to the best site of care within the system. But for independent, and particularly smaller and rural hospitals, the process of finding an accepting hospital for patients needing transfer is a huge burden that involves placing one phone call or digital request at a time. Once a patient is accepted somewhere, the facility must then begin the process of finding a transport resource, coordinating the right time of transfer with the receiving facility, and completing the required documentation.
This points to a need for centers that may specialize in regional patient movement, to include all hospitals and systems. In regions like San Antonio, Texas, this innovation has taken place already and serves needs across a large geographic region and many patient types (https://www.strac.org/). The state of Georgia has developed and funded a coordinating center for patient movement and EMS communications on hospital capabilities (https://georgiarcc.org/). These coordinating centers have been advantageous when patient surges occurred, such as those experienced during the most stressful days of the COVID-19 pandemic.
Emergency physicians have ongoing leadership opportunities in changing and regionalizing the acute care delivery system. The need to serve ED patients who must be transferred for ongoing care is an important management priority that was recognized widely during the pandemic and will continue into the future.
 Dr. Augustine is a member of the ACEP Now Editorial Board; Clinical Professor of Emergency Medicine at Wright State University in Dayton, Ohio; and Vice President of the Emergency Department Benchmarking Alliance.
Dr. Augustine is a member of the ACEP Now Editorial Board; Clinical Professor of Emergency Medicine at Wright State University in Dayton, Ohio; and Vice President of the Emergency Department Benchmarking Alliance.
References
- Augustine JJ. Another COVID casualty: The emergency
department transfer process. ACEP Now. 2022;41(2):15.
- Sarzynski SH, Mancera AG, Yek C, et al. Trends in patient transfers from overall and caseload-strained US hospitals during the COVID-19 pandemic. JAMA Netw Open. 2024;7(2):e2356174. doi:10.1001/jamanetworkopen. 2023.56174
- Augustine JJ. A sobering year for EDs and their patients. ACEP Now. 2023;42(12):19.
Pages: 1 2 3 | Multi-Page






No Responses to “Interhospital Transfer Capabilities Still Pose Major Issues”