Results
Explore This Issue
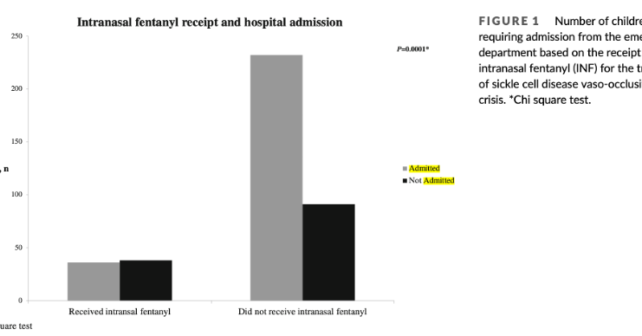
ACEP Now: Vol 42 – No 09 – September 2023They included 400 patients with 54 percent being female. The median age was 15 years. Most patients (92 percent) had hemoglobin SS disease while the other eight percent had hemoglobin S-beta thalassemia. The overall rate of admission was 67 percent. In this study 19 percent of SCD with VOE received IN fentanyl.
Key Results
IN fentanyl use was associated with greater odds of being discharged from the ED in children with SCD and VOE compared to those who did not receive IN fentanyl.
Primary Outcome: Discharged home from the ED
Secondary Outcomes: There were several secondary outcomes. Two interesting findings were time to parenteral opioid administration and total dose of opioid morphine equivalents. Those who received IN fentanyl had a much greater odds ratio of receiving parenteral opioid within 30 and 60 minutes and received greater amounts of opioids:
≤30 minutes: OR, 9.38; 95 percent CI, 5.22-16.83
≤60 minutes: OR, 9.83; 95 percent CI, 4.87-19.85
Total morphine equivalents IN fentanyl 0.36 mg/kg (SD, 0.14) versus no IN fentanyl 0.22 mg/kg (SD, 0.25)
EBM Commentary
Selection Bias: Investigators from each site reviewed 20 consecutive charts. The annual ED volume of patients with SCD VOE ranged from 80 to 700 per year. It is unclear exactly how the 20 charts were selected for evaluation and if they accurately represented the overall population of SCD patients that sought care for VOE. This opens the potential for selection bias being introduced into the data set.
Time and Dose of Opioid Administration: Children who received IN fentanyl received their first dose of parenteral opioid significantly faster compared to the children who did not. It’s possible that the faster administration of opioid therapy in general plays a bigger role in ability to discharge a SCD patient with VOE than the administration of IN fentanyl. However, the multivariable analysis did not find that timeliness of opioid administration was associated with decreased odds of hospital admission.
Another interesting secondary outcome that could confound the results is that children who received IN fentanyl received higher overall total parenteral opioid morphine equivalents. We would have thought those receiving pain medicine faster would lead to a lower overall total amount of parenteral opioids being used.
External Validity: In this study, 15 out of 20 sites had the ability to administer IN fentanyl. Out of those 15 sites, only 10 sites administered IN fentanyl. Was the use of IN fentanyl simply not part of the institutional culture or not a standardized pathway for treating VOE? Or perhaps patient preferences played a role and IN fentanyl was offered but declined.
Pages: 1 2 3 | Single Page




No Responses to “Intranasal Fentanyl for Sickle Cell Vaso-Occlusive Pain”