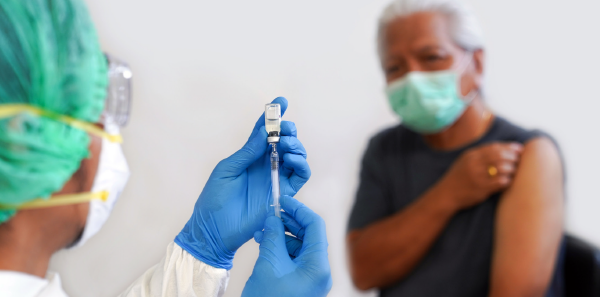
The COVID-19 pandemic has proven, yet again, that U.S. emergency departments are a critical part of the nation’s health care safety net. As medical centers throughout the country canceled visits in the spring and shifted ambulatory visits to telemedicine, emergency departments remained open and continued to provide 24-7 care. As the coronavirus surges across the nation, emergency departments will continue to care for patients who might otherwise not have in-person contact with the health care system. Emergency departments represent a critical component of the health care infrastructure. There is a unique opportunity for them to serve individual patients, meet public health needs, and contribute to the integrity of the health care system itself by helping to maintain hospital capacity: by providing coronavirus vaccinations during acute ED patient encounters in appropriately selected patients.
Explore This Issue
ACEP Now: Vol 40 – No 02 – February 2021Approach to ED-Based Coronavirus Vaccination
Pilot programs across the country have demonstrated over several years the viability of using the emergency department to bolster influenza vaccinations programs.1–4 However, there has not been broad uptake of these programs, despite policy statements supporting such programs from national organizations including the Centers for Disease Control and Prevention, Advisory Committee on Immunization Practices, and ACEP itself. With the need to vaccinate millions of people across the country against SARS-CoV-2, now is the right time for U.S. emergency departments to consider implementing vaccination programs.
In 2016, there were 144.8 million ED visits in the United States.5 Compared to the rest of the health care system, individuals who visit emergency departments are disproportionately minorities, less likely to have other contacts with the health care system, and less likely to have health insurance. Thus, we can surmise lower vaccination rates among ED patients compared to the overall U.S. population. These same communities have been disproportionally affected by the COVID-19 pandemic and would most benefit from widespread vaccination efforts.
Why EDs?
Every year, hospitalizations, ambulance diversion, and overall demand on ED resources increase in the winter months, partially driven by the influenza season.6 Hospital systems nationwide are more concerned than ever about inpatient capacity in light of the COVID-19 pandemic. Vaccinating their communities against influenza and SARS-CoV-2 may ease strains on hospital capacity by preventing cases of influenza and COVID-19 that would otherwise present to the emergency departments and potentially require admission.
Detractors may suggest that emergency departments should not engage in public health initiatives, as they can be costly, interfere with ED throughput, and interfere with our primary mission to provide emergent care. However, prior work by the Emergency Medicine Transmissible Infectious Diseases and Epidemics interest group of the Society for Academic Emergency Medicine on HIV testing in emergency departments has demonstrated emergency departments can facilitate public health initiatives while continuing to provide high-quality care without negatively affecting patient throughput or health system costs.7,8 Success of this endeavor will require partnership and sharing/diversion of personnel, resources, and infrastructure from local, state, regional, and federal partners.
Emergency departments can be part of the solution to a vast health care problem that includes reaching out to the underserved, uninsured, and minority patients who we need to help get vaccinated against SARS-CoV-2. We believe that because we can, we have an obligation to do so. As a specialty, we pride ourselves on our ability to be versatile and adapt to whatever catastrophes the world throws our way. Embracing imperatives such as this proves our adaptability in the face of a pandemic and may even lead to the enhancement of the prestige of our specialty.
Disclosures: Dr. Lyons receives investigator-initiated project support from Gilead Sciences, Inc. paid to the institution. Dr. Wilson receives grant support from Gilead Pharmaceuticals, Alexion, Janssen, and Pfizer.
Originally published in SAEM Pulse Jan.–Feb. 2021.
Dr. Schechter-Perkins is with Boston University School of Medicine/Boston Medical Center. Dr. Rothman, Dr. Hansoti, Dr. Hsieh, and Dr. Klein are with John Hopkins University School of Medicine in Baltimore. Dr. Faryar and Dr. Lyons are with University of Cincinnati College of Medicine. Dr. Waxman is with Albany Medical College in Albany, New York. Dr. May is with UC Davis Health in Sacramento, California. Dr. Wilson is with Morsani College of Medicine, University of South Florida, Tampa General Hospital. Dr. Martin is with Ohio State University Wexner Medical Center in Columbus. All are members of the EMTIDE interest group.
References
- Rodriguez RM, Baraff LJ. Emergency department immunization of the elderly with pneumococcal and influenza vaccines. Ann Emerg Med. 1993;22(11):1729-1732.
- Slobodkin D, Kitlas J, Zielske P. Opportunities not missed—systematic influenza and pneumococcal immunization in a public inner-city emergency department. Vaccine. 1998;16(19):1795-1802.
- Rimple D, Weiss SJ, Brett M, et al. An emergency department–based vaccination program: overcoming the barriers for adults at high risk for vaccine-preventable diseases. Acad Emerg Med. 2006;13(9):922-930.
- Casalino E, Ghazali A, Bouzid D, et al. Emergency department influenza vaccination campaign allows increasing influenza vaccination coverage without disrupting time interval quality indicators. Intern Emerg Med. 2018;13(5):673-678.
- Lane BH, Mallow PJ, Hooker MB, et al. Trends in United States emergency department visits and associated charges from 2010 to 2016. Am J Emerg Med. 2020;38(8):1576-1581.
- Schull MJ, Mamdani MM, Fang J. Community influenza outbreaks and emergency department ambulance diversion. Ann Emerg Med. 2004;44(1):61-67.
- Kecojevic A, Lindsell CJ, Lyons MS, et al. Public health and clinical impact of increasing emergency department–based HIV testing: perspectives from the 2007 conference of the National Emergency Department HIV Testing Consortium. Ann Emerg Med. 2011;58(1 Suppl 1):S151-S159.e1.
- Galbraith JW, Anderson ES, Hsieh Y-H, et al. High prevalence of hepatitis C infection among adult patients at four urban emergency departments—Birmingham, Oakland, Baltimore, and Boston, 2015–2017. MMWR Morb Mortal Wkly Rep. 2020;69(19):569-574.
Pages: 1 2 | Multi-Page




No Responses to “Opinion: Let’s Give Vaccination Programs a Shot”