Explore This Issue
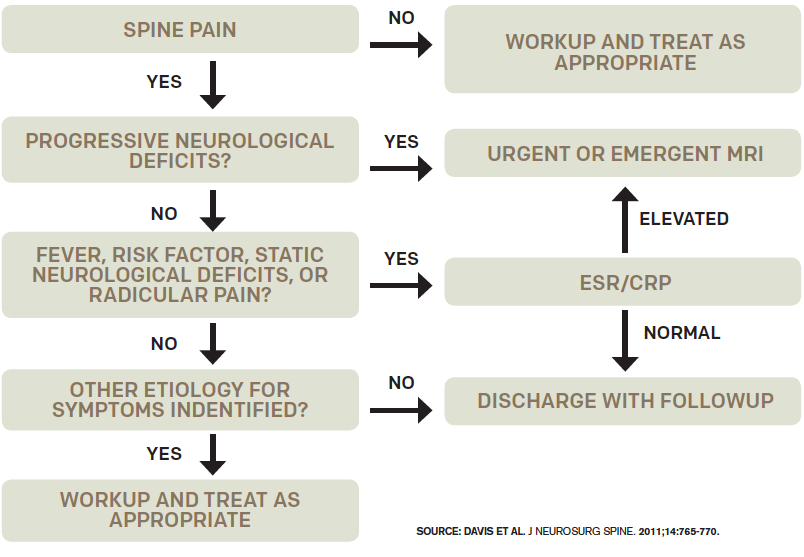
ACEP Now: Vol 36 – No 01 – January 2017Figure 1: Decision guideline for diagnosing spinal epidural abscess.
C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) may help in deciding whether to pursue an MRI, depending on the clinical suspicion for epidural abscess (see Figure 1). In one study, 98 percent of patients with epidural abscess had an ESR >20.3 If suspicion is low after the history and physical, low ESR and CRP levels support not doing an MRI, and discharging the patient home with close follow-up is appropriate. ESR is also helpful for predicing prognosis in patients with spinal metastasis. If there is a high index of suspicion for cord compression, an MRI is indicated regardless of CRP or ESR. See Figure 2 for an algorithm for managing non-traumatic back pain.

Figure 2. Algorithm for management of nontraumatic back pain.
Solid lines indicate usual care; dotted lines indicate options based on case-by-case clinical judgment.
Credit: Reprinted with permission from Ann Emerg Med. 2015;66:148-153.
One of the most common pitfalls in working up the patient suspected of spinal infection, and a good example of the cognitive bias of premature closure, is finding osteomyelitis on CT scan and stopping there. CT cannot rule out a concomitant epidural abscess, which requires urgent surgical decompression, because it does not show the epidural space, spinal cord, or spinal nerves adequately. Another common imaging pitfall is not imaging the entire spine when epidural abscess is being considered. Remember, if the suspicion is epidural abscess or spinal metastasis, the entire spine must be imaged by MRI.
So next time you see patients with low back pain in the emergency department on their third visit for the same illness, consider the big five diagnoses; employ cognitive forcing strategies; ask about risk factors and red flags; assess the posture of sciatica patients; perform a careful exam for saddle anesthesia; consider a post-void residual, CRP, and/or ESR; and obtain an MRI of the entire spine for suspected spinal infection or spinal metastases. Your patients will thank you, and you may stay out of court.
A special thanks to Dr. Walter Himmel and Dr. Brian Steinhart for their participation in the EM Cases podcast from which this article is based.
 Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
Resource from Emergency Medicine Cases Website
Podcast- Episode 26: Low Back Pain Emergencies (emergencymedicinecases.com/episode-26-low-back-pain-emergencies/). You can also add EM Cases to your podcast app via emergencymedicinecases.com/casting-setup.
Pages: 1 2 3 | Single Page




2 Responses to “Low Back Pain Emergencies Could Signal Neurological Injuries”
March 1, 2020
Steven Shroyer MD FACEPNice review Dr Hellman. If I could add, more recent literature including the two your referenced by D Davis 2004 and 2011 warn not to wait for back pain and fever, since this will miss the majority of spinal infections. Both of these articles indicate only 24% (2004 JEM) and 7% (2011 JNS)of spinal infections had fever >= 100.4 degrees F. Also these two articles indicate 100% of spinal infections had one or more risk factors–much more sensitive than fever. Thanks for the article. Steve
January 11, 2025
Chijioke OtikpaWonderful document! But discussing non specific low back pain management while carefully avoiding any mention of physical therapy is WILD!
So there’s no PT referral plan at any point?