The two most common side effects that do occur are dizziness and mild dysphoria, sometimes referred to as psychotomimetic reactions. Mild dysphoric events are far shorter and less severe than true emergence reactions.6 The incidence of these ranges from 3 percent to 15 percent, depending on the study’s definition, reporting, and dose.2,4,6 They typically occur immediately after administration and quickly resolve. An approach where the patient receives a short explanation of the drug’s occasional tendency to cause brief feelings of unreality has, anecdotally, reduced the incidence of dysphoric reactions.5,6 This is likely because patients who expect such feelings are far less alarmed when they do occur and view them as a brief side effect rather than an unexpected event that could portend an unintentional overdose. Interestingly, a recent study compared LDK intravenous push over 5 minutes to a 15-minute short infusion in 100 mL of normal saline; dysphoria was significantly reduced in the short infusion group, while no differences were seen in analgesia. This would seem to confirm the anecdotal experience that slower administration decreases side effects.9
Explore This Issue
ACEP Now: Vol 36 – No 08 – August 2017Dizziness is, by far, the most common adverse drug event, reported in roughly 20 percent of patients in randomized controlled trials polling patients about side effects.4 Generally, this incidence increases in a dose-dependent fashion in the literature. However, this may have as much to do with differing trial designs as it does with drug effects.
In one large (n=530), retrospective, consecutive case series, 6 percent of patients experienced an adverse event documented in the chart.6 Seven patients (1.5 percent) developed transient hypoxia. Four of those also received hydromorphone, and all but one (chronic obstructive pulmonary disease requiring bilevel positive airway pressure) resolved with 2 L of oxygen via nasal cannula. Eighteen patients (3.5 percent) developed psychotomimetic/dysphoric disturbances, but only three received benzodiazepines. The disposition was unaltered in all. Five patients (1 percent) experienced emesis. While this study was limited by its retrospective design, its strength is that, presumably, only clinically relevant adverse drug events were documented. Most important, any incidents of true emergence phenomenon, laryngospasm, apnea, or cardiac arrest would certainly have been detected if they occurred. None were detected in this or any other study.6
Discussion
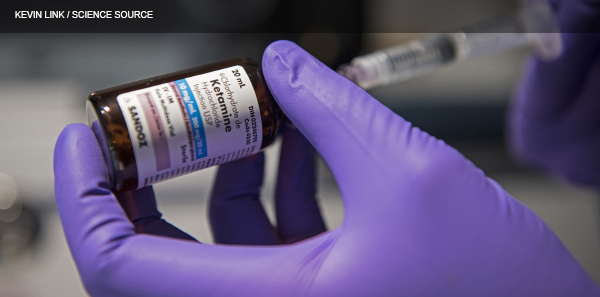
A comprehensive review of the literature reveals that LDK is safe to use. It is most efficacious between 0.15 and 0.30 mg/kg as an intravenous push, but slow infusions show promise. More than 10 studies, not all reviewed here, uniformly demonstrate that LDK is noninferior to morphine when compared head-to-head. Benign side effects are common and include dizziness and dysphoria, as opposed to the nausea and respiratory depression seen from morphine. LDK is indicated any time patients are in pain but is especially appropriate for opioid-tolerant patients, recovering addicts, or patients with a tenuous respiratory status or hypotension. Because of LDK’s opiate-potentiating effects, it is also appropriate and safe to use in patients with acute pain refractory to opioid treatment.4
Pages: 1 2 3 | Single Page




5 Responses to “Low-Dose Ketamine Emerges as Effective Opioid Alternative”
August 21, 2017
Dr. Chuck SwansonI used to live to use it. Would still use it, but in Mississippi ER nurses are not not allowed to monitor patients that have been given moderate sedation. New head of Nursing Board is a NA and made ruling. I work in 2 smaller ERs and it has hampered our ability to care for patients. Can give Versed, a BZD and Fentanyl. Sucks
September 9, 2017
Gabe WilsonChuck,
This same issue crops up all over. The key is, this is not moderate sedation. This is analgesia. In the past Ketamine was only used for sedation so the thought process is locked into using at such.
Change the thinking.
Share the evidence.
In the end, low dose ketamine is much safer the hydromorphone or many of the alternatives.
September 5, 2017
Laura QuintThe bigger issue with ketamine as an analgesic is it’s use outside of the ED – it is all very well if you can discharge home after using but if being admitted you risk misaligned expectations from the patient.
Many places only approve low dose ketamine in the ED, ICU and occasionally the OR/PACU.
What about everyone else?
January 6, 2020
Arnold MillerAny body have experience with using LDK for migraines for heavily pretreated patients?
January 15, 2021
Michelle CostelloSounds quite interesting
Many pain relievets
Are hard on kidneys
And often not effective
Long term
Very interesting