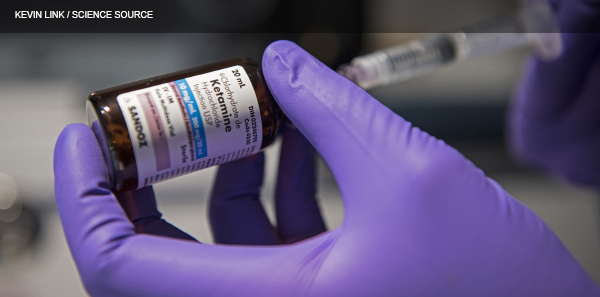
Amid a national opioid epidemic, there is a search for other effective analgesics in the emergency department, both to avoid providing a “fix” as well as to avoid the dangerous side effects of opioids. Recently, ketamine has begun to answer this need. When used at doses greater than 1 mg/kg IV, ketamine has amnestic, sedative, and profound analgesic properties. However, recent research indicates that ketamine’s analgesic properties remain at significantly lower doses. In fact, one review of combat analgesia in the US military characterized ketamine as “an almost ideal analgesic because of its profound pain relief, its potentiation of opioids, its role in preventing opioid hyperalgesia, and its large margin of safety.”1 This article explores the evidence for low-dose ketamine (LDK) for analgesia in the emergency department.
Explore This Issue
ACEP Now: Vol 36 – No 08 – August 2017Efficacy of Analgesia
LDK has been shown to decrease pain scores, both in conjunction with morphine and as a stand-alone treatment.2–5 It is noninferior to morphine when used alone at doses of 0.15 or 0.3 mg/kg. Effective analgesia occurs within minutes and lasts roughly 90 minutes.4 LDK potentiates the effects of morphine and has been uniformly shown to reduce required doses of morphine when administered together.2 Two studies found that 67 percent and 85 percent of patients receiving LDK would like to receive it again for similar pain.3,5
Dosing
Given the markedly different effects between ketamine dosed at dissociative and analgesic doses, attention to dosing is crucial. LDK has been studied from 0.1–0.3 mg/kg, with some studies using a uniform 10 mg or 15 mg dose. Most controlled studies dose ketamine at 0.15 or 0.3 mg/kg as these doses are well-studied in the postoperative anesthesia literature, and this dose range is appropriate for ED use.2 Whether weight-based dosing is required or a uniform dose is acceptable remains unclear. Ahern and colleagues followed initial doses with a 20 mg/hour infusion, which appeared to be superior to push-dose-only LDK, although there was no control group.3
Ketamine is sometimes used as a street drug, and recreational effects traditionally start around 0.4 mg/kg, so higher dosing runs the risk of placing your patient in a psychedelic state, where they may experience some hallucinations or even a partially dissociated state that can be quite distressing to those not seeking that experience.
A large-scale, double-blind, randomized, controlled trial is still needed to effectively determine an optimal dose, whether weight-based dosing is required, and what rate of continuous infusion should be used.
Side Effects
There is a major disconnect between physicians’ perceptions of LDK side effects and reality. In fact, anticipation of emergence reactions is the number-one reason physicians fear the use of LDK in the emergency department.5 However, emergence reactions are nearly impossible with properly dosed LDK, and no true emergence reactions were reported in any study evaluating LDK.2–6 Another common fear of ketamine use is elevation of intracranial pressure (ICP). However, ketamine does not increase ICP even at dissociative doses.7 Furthermore, it does not inhibit respiratory drive to the point of apnea at analgesic doses and only rarely in procedural sedation doses.8 Up to hundredfold (50 mg/kg) overdoses have been reported with no adverse events other than prolonged, otherwise typical sedation.4,8
The two most common side effects that do occur are dizziness and mild dysphoria, sometimes referred to as psychotomimetic reactions. Mild dysphoric events are far shorter and less severe than true emergence reactions.6 The incidence of these ranges from 3 percent to 15 percent, depending on the study’s definition, reporting, and dose.2,4,6 They typically occur immediately after administration and quickly resolve. An approach where the patient receives a short explanation of the drug’s occasional tendency to cause brief feelings of unreality has, anecdotally, reduced the incidence of dysphoric reactions.5,6 This is likely because patients who expect such feelings are far less alarmed when they do occur and view them as a brief side effect rather than an unexpected event that could portend an unintentional overdose. Interestingly, a recent study compared LDK intravenous push over 5 minutes to a 15-minute short infusion in 100 mL of normal saline; dysphoria was significantly reduced in the short infusion group, while no differences were seen in analgesia. This would seem to confirm the anecdotal experience that slower administration decreases side effects.9
Dizziness is, by far, the most common adverse drug event, reported in roughly 20 percent of patients in randomized controlled trials polling patients about side effects.4 Generally, this incidence increases in a dose-dependent fashion in the literature. However, this may have as much to do with differing trial designs as it does with drug effects.
In one large (n=530), retrospective, consecutive case series, 6 percent of patients experienced an adverse event documented in the chart.6 Seven patients (1.5 percent) developed transient hypoxia. Four of those also received hydromorphone, and all but one (chronic obstructive pulmonary disease requiring bilevel positive airway pressure) resolved with 2 L of oxygen via nasal cannula. Eighteen patients (3.5 percent) developed psychotomimetic/dysphoric disturbances, but only three received benzodiazepines. The disposition was unaltered in all. Five patients (1 percent) experienced emesis. While this study was limited by its retrospective design, its strength is that, presumably, only clinically relevant adverse drug events were documented. Most important, any incidents of true emergence phenomenon, laryngospasm, apnea, or cardiac arrest would certainly have been detected if they occurred. None were detected in this or any other study.6
Discussion
A comprehensive review of the literature reveals that LDK is safe to use. It is most efficacious between 0.15 and 0.30 mg/kg as an intravenous push, but slow infusions show promise. More than 10 studies, not all reviewed here, uniformly demonstrate that LDK is noninferior to morphine when compared head-to-head. Benign side effects are common and include dizziness and dysphoria, as opposed to the nausea and respiratory depression seen from morphine. LDK is indicated any time patients are in pain but is especially appropriate for opioid-tolerant patients, recovering addicts, or patients with a tenuous respiratory status or hypotension. Because of LDK’s opiate-potentiating effects, it is also appropriate and safe to use in patients with acute pain refractory to opioid treatment.4
 Dr. Smith is chief resident at the Sinai-Grace Hospital emergency medicine residency program at Wayne State University School of Medicine in Detroit.
Dr. Smith is chief resident at the Sinai-Grace Hospital emergency medicine residency program at Wayne State University School of Medicine in Detroit.
 Dr. Messman is the associate program director of the Sinai-Grace Hospital emergency medicine residency program and assistant professor at Wayne State University School of Medicine.
Dr. Messman is the associate program director of the Sinai-Grace Hospital emergency medicine residency program and assistant professor at Wayne State University School of Medicine.
 Dr. Wilburn is faculty in the Sinai-Grace Hospital emergency medicine residency program and assistant professor at Wayne State University School of Medicine.
Dr. Wilburn is faculty in the Sinai-Grace Hospital emergency medicine residency program and assistant professor at Wayne State University School of Medicine.
References
- Black IH, McManus J. Pain management in current combat operations. Prehosp Emerg Care. 2008;13(2):223-227.
- Beaudoin FL, Lin C, Guan W, et al. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double-blind, clinical trial. Acad Emerg Med. 2014;21(11):1193-1202.
- Ahern TL, Herring AA, Miller S, et al. Low-dose ketamine infusion for emergency department patients with severe pain. Pain Med. 2015;16(7):1402-1409.
- Miller JP, Schauer SG, Ganem VJ, et al. Low-dose ketamine vs morphine for acute pain in the ED: a randomized controlled trial. Am J Emerg Med. 2015;33(3):402-408.
- Richards JR, Rockford RE. Low-dose ketamine analgesia: patient and physician experience in the ED. Am J Emerg Med. 2013;31(2):390-394.
- Ahern TL, Herring AA, Anderson ES, et al. The first 500: initial experience with widespread use of low-dose ketamine for acute pain management in the ED. Am J Emerg Med. 2015;33(2):197-201.
- Cohen L, Athaide V, Wickham ME, et al. The effect of ketamine on intracranial and cerebral perfusion pressure and health outcomes: a systematic review. Ann Emerg Med. 2015;65(1):43-51.e2.
- Green SM, Clark R, Hostetler MA, et al. Inadvertent ketamine overdose in children: clinical manifestations and outcome. Ann Emerg Med. 1999;34(4 Pt 1):492-497.
- Motov S, Mai M, Pushkar I, et al. A prospective randomized, double-dummy trial comparing intravenous push dose of low dose ketamine to short infusion of low dose ketamine for treatment of moderate to severe pain in the emergency department [published online ahead of print March 3, 2017]. Am J Emerg Med.
Pages: 1 2 3 | Multi-Page




5 Responses to “Low-Dose Ketamine Emerges as Effective Opioid Alternative”
August 21, 2017
Dr. Chuck SwansonI used to live to use it. Would still use it, but in Mississippi ER nurses are not not allowed to monitor patients that have been given moderate sedation. New head of Nursing Board is a NA and made ruling. I work in 2 smaller ERs and it has hampered our ability to care for patients. Can give Versed, a BZD and Fentanyl. Sucks
September 9, 2017
Gabe WilsonChuck,
This same issue crops up all over. The key is, this is not moderate sedation. This is analgesia. In the past Ketamine was only used for sedation so the thought process is locked into using at such.
Change the thinking.
Share the evidence.
In the end, low dose ketamine is much safer the hydromorphone or many of the alternatives.
September 5, 2017
Laura QuintThe bigger issue with ketamine as an analgesic is it’s use outside of the ED – it is all very well if you can discharge home after using but if being admitted you risk misaligned expectations from the patient.
Many places only approve low dose ketamine in the ED, ICU and occasionally the OR/PACU.
What about everyone else?
January 6, 2020
Arnold MillerAny body have experience with using LDK for migraines for heavily pretreated patients?
January 15, 2021
Michelle CostelloSounds quite interesting
Many pain relievets
Are hard on kidneys
And often not effective
Long term
Very interesting