Tips on sternal stabilization, making vertical and horizontal incisions, palpitating the cricothyroid membrane from an emergency physician
Explore This Issue
ACEP Now: Vol 33 – No 04 – April 2014Part one of this article addressed the “laryngeal handshake,” a means of reliably finding the external landmarks for performing a cricothyrotomy. We left off with the nondominant hand stabilizing the larynx, and the dominant hand resting on the sternum. “Sternal stabilization” is fundamental for good control of the scalpel. By firmly pushing your dominant hand against the patient’s sternum, your hand is not hovering in space over the neck. It also helps tremendously when your elevated heart rate would otherwise impede fine motor control. The blade needs to be controlled two ways: first, for the midline vertical incision through the skin and, second, rotating the blade for the horizontal incision through the cricothyroid membrane.
Breaking down the sequential steps:
- Laryngeal handshake, nondominant hand on larynx (see Figure 1)
- Sternal stabilization (dominant hand on sternum)
- Vertical skin incision
- Palpation of the cricothyroid membrane with the nondominant index finger
- Horizontal incision through the membrane
- Flip the blade (extending the incision) in the other direction
Although single stab incisions through the skin and membrane are feasible in thin individuals, a vertical skin incision is best. A skin incision permits direct palpation of the cartilages and cricothyroid membrane, confirming the correct location before making the horizontal incision into the airway (see Figure 2). In the super obese, larger vertical incisions are required to enable the horizontal incision.

Figure 1.
The “laryngeal handshake,” from left to right:
1) hyoid,
2) thyroid,
3) cricoid, and 4) palpation of cricothyroid membrane.

Figure 2.
Making the initial vertical skin
incision.

Figure 3.
Palpating the cricothyroid membrane.
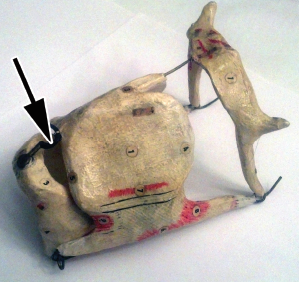
Figure 4. The “cartilaginous cage” (arrow) on a papier-mâche model of the laryngeal cartilages. Produced by Dr. Louis Auzoux, Paris, France, circa 1850. Collection of Richard M. Levitan, MD.
The importance of verifying the cricothyroid membrane cannot be overstated. At this location, the incision has protected boundaries created by what I call the “cartilaginous cage” (see Figures 3 and 4). This is a “safe space” delineated by cartilage: above is the inferior aspect of the thyroid lamina; below is the anterior cricoid ring; laterally are the inferior cornu of the thyroid (on either side); and, perhaps most important, there is a firm backstop, the high back wall of the cricoid cartilage (see Figure 5). If the incision is made too high (between the hyoid and thyroid), it will be above the vocal cords. If made too low (below the cricoid) you enter the trachea. At the trachea, there is nothing stopping the blade from going too far laterally (i.e., cutting great vessels) and also nothing to prevent puncturing the posterior membranous trachea (entering the esophagus and mediastinum).

Figure 6. Inserting a Shiley. Initial tip insertion is made 90 degrees to the tracheal axis, and then after the tip has passed, the device is rotated in the direction of the tracheal axis on full insertion.
A tracheal hook has a sharp point to puncture the membrane and lift up on the inferior thyroid, stabilizing the trachea while the incision is performed. Whether or not a hook is used, when using a #11 blade, it’s necessary to widen the incision by extending the cut in the other direction after the blade enters the trachea. A #10 blade, because it has a larger width, may not require this. If a hook is not used to control the trachea, something should go immediately into the hole. A finger, the back end of the scalpel, or a bougie all have been recommended for this task. A tracheal hook can also be used at this stage, after the hole has been made, to control and lift up the trachea.
Bougie advocates claim it can confirm placement by depth of insertion (e.g., if in the trachea, it will advance considerably). A tube can then be railroaded over it once you know the bougie is in the correct place.
It is far easier to insert a standard tube (6-0 ID, OD 8.2 mm) than a Shiley into the cricothyroid membrane. Its flexibility and smaller size allow for easy insertion, but one has to watch the depth of placement. It is only 11 cm from the cords to the carina. Most pilot balloons on a tracheal tube are at about 14 mm from the tip. Overinsertion will lead to right main-stem intubation. A 6-0 Shiley has an OD of 10.8 mm, while the cricothryoid membrane has a height ranging from 8–11 mm (females to males). Shileys are also mechanically harder to insert because they must be rotated into position. Initially, they should be 90 degrees to the tracheal axis, and after the tip is placed into the hole, the back end is swung around to be in line with the tracheal axis as it is fully inserted (see Figure 6).
The surgical airway is one of the most intimidating procedures for emergency physicians. The “laryngeal handshake,” “sternal stabilization,” and appreciating the “cartilaginous cage” can make you perform like a hero in the crisis moment when your patient needs a cric.
 Dr. Levitan is an adjunct professor of emergency medicine at Dartmouth’s Geisel School of Medicine in Hanover, N.H., and a visiting professor of emergency medicine at the University of Maryland in Baltimore. He works clinically at a critical care access hospital in rural New Hampshire and teaches cadaveric and fiber-optic airway courses.
Dr. Levitan is an adjunct professor of emergency medicine at Dartmouth’s Geisel School of Medicine in Hanover, N.H., and a visiting professor of emergency medicine at the University of Maryland in Baltimore. He works clinically at a critical care access hospital in rural New Hampshire and teaches cadaveric and fiber-optic airway courses.
Pages: 1 2 3 | Multi-Page





3 Responses to “How to Make the Incision, Insert the Tube in Cricothyrotomy”
April 27, 2014
DavidGood review. I like the catch phrases used. Gives good small tasks to focus on when in a stressful situation.
One question: the article says “It is only 11 mm from the cords to the carina”. Should be cm, yes? Regardless, the point made is well taken: don’t over insert an endotracheal tube.
May 5, 2014
Dawn Antoline-WangThank you for the comment. You’re right, the article should read 11 cm. We have corrected the error.
June 22, 2014
dskibbieA great article. My only concern is that using an ET tube for cricothyrotomy means that ANOTHER critical procedure is necessary, as the ET tube is not particularly stable. There are short tubes which are not nearly as thick as a shiley available. We use the Chinook kit for our air bases. It’s cheap and effective. It also works well with a bougie guided procedure. I’m sure there are other purpose designed crico tubes out there, and I am not affiliated with the maker. The other alternative is to use a 4 shiley.
Thanks!