
Emergency physicians are proficient in recognizing and caring for the dying medical or trauma patient but often have limited training in managing patients who are actively dying from a terminal illness, organ failure, or frailty.1 These patients frequently present to emergency departments and have a predictable set of symptoms that can be managed. Emergency physicians should understand the treatments available and how to use them for patients arriving from hospice or transitioning to comfort care in the emergency department. This article will review the recommended medical treatments for patients requiring end-of-life comfort care in the emergency department.
Explore This Issue
ACEP Now: Vol 40 – No 07 – July 2021When choosing medications to address symptomatic care in the acutely dying patient, emergency physicians should take into account half-life, dosing, route, and onset of action. It is important to consider whether the patient has already been receiving these medications prior to arrival; if not, multiple doses may be necessary to achieve symptom relief. The intravenous route is preferred, as it is easily titratable with a fast onset. However, buccal, nasal, subcutaneous, oral, and intramuscular routes are also frequently acceptable.2–4 See Table 1 for a summary of palliative medical management options for various symptoms.
The Case
A 56-year-old male with end-stage pancreatic cancer is brought to your emergency department after his partner was unable to control his symptoms with his prescribed pain regimen. He arrives complaining of diffuse abdominal pain and shortness of breath.
Vitals:
- Temperature: 98º F
- Heart rate: 105
- Blood pressure: 110/55
- Respiratory rate: 29
- Oxygen saturation: 95 percent
Physical exam is significant for a distended abdomen with diffuse moderate abdominal tenderness with nausea. He is short of breath. He and his partner understand that his cancer is terminal and are ready for home hospice. Hospice staff will arrive in the morning, but the pain and discomfort are unbearable now.
How will you provide aggressive palliative resuscitation in the emergency department until the hospice team arrives in the morning?
Dyspnea
Dyspnea is prevalent in terminally ill patients and is a frequently distressing symptom that drives patients to the emergency department at the end of life. Opioids are the first-line treatment for palliation of dyspnea.5 They decrease the chemoreceptor response to hypercapnia, thereby depressing the central respiratory drive and mitigating anxiety.5 In the opioid-naive patient, low doses of oral or IV morphine can provide relief. In patients who are already taking opioids regularly, administer 5 percent of their total daily morphine dose to manage dyspnea.2–4 Oxycodone or hydromorphone can also be used, particularly in patients with a morphine allergy.
Other nonpharmacological alternatives include positioning a fan to blow cool air toward the face, repositioning the patient for better oxygenation, and administering supplemental oxygen.2–4 Admission to the hospital or hospice inpatient unit should be considered when a patient is experiencing refractory dyspnea despite initial palliative resuscitation with appropriate medications, alternative medical interventions, and the ruling out of any reversible causes of dyspnea. Management of a terminally ill patient with refractory symptoms should be escalated to a palliative physician for reassessment of end-of-life care in an acute setting.
Pain
Opioids are also the principal treatment for pain in terminally ill patients. Intravenous administration of opioids is generally best for controlling severe nociceptive pain that is new or escalating, whereas oral medication can be better for chronic mild or moderate pain if the patient tolerates oral administration.2–4 Given the rapid peak plasma concentration (six minutes) and short half-life of IV opioids, patients should be reassessed every 15 minutes for repeated doses. The half-life of morphine and hydromorphone is approximately two hours. The duration of action of fentanyl is only 30 minutes to an hour.6
When assessing a patient who presents to the emergency department with an acute pain exacerbation despite the use of their home medications, emergency physicians should calculate the 24-hour dose of their prescribed opioids and use an equianalgesic dosage conversion calculator so the patient is appropriately medicated. When converting from an oral morphine equivalent to another opioid in a patient with a high opioid requirement, emergency physicians should reduce the total dosage of the new opioid medication by 25 to 50 percent. Be cautious in terminally ill patients who may have renal impairment and avoid morphine, as this can lead to opioid-induced neurotoxicity. Use hydromorphone or fentanyl as the opioid of choice if there is known renal impairment.
Infusions Versus Push Dose IV
The dose of opioids for pain management in the dying patient should be increased by 50 to 100 percent regardless of the starting dose until pain is adequately controlled. Infusions are less effective in the short-term emergency setting, as they require four to five half-lives to reach steady plasma concentration, which can take up to 10 hours.6 Bolus doses outlined in Table 1 are recommended, and infusions can be considered as a supplement if long-term pain management is necessary.
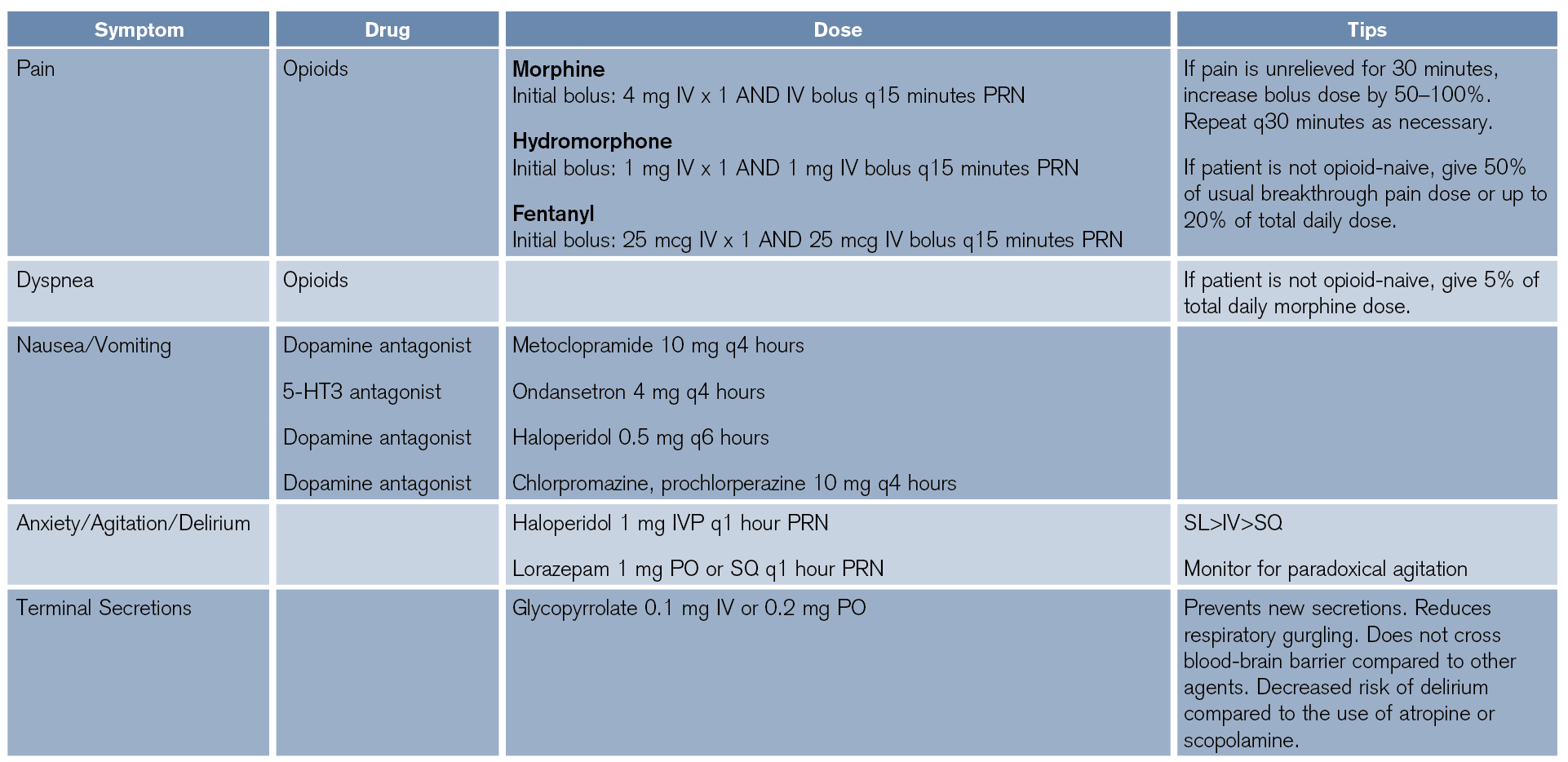
(click for larger image) Table 1: Palliative Medical Management of Symptoms in the Acutely Dying Patient
The Principle of Double Effect
The “principle of double effect” is an ethical doctrine that indicates that an action with both intended and unintended outcomes is justified if the intended benefit significantly outweighs the unintended harm.7 This has historically been applicable to the concern that opioids may depress respiratory drive and therefore accelerate the dying process. While the use of opioids is widely considered justified by the principle of double effect, there is evidence that opioids do not actually hasten death when used appropriately for pain in the actively dying patient, particularly at low doses.8–10 One study found that opioid use titrated to comfort in a palliative setting does not significantly alter PaCO2, PaO2, or overall survival. It does, however, manage pain and reduce dyspnea, thereby significantly increasing comfort at the end of life.1,9,10
One notable exception of the double effect is in conscious patients with imminent airway loss. These patients require rapid and large boluses of opioids or benzodiazepines, propofol, ketamine, barbiturate, etc. The ultimate result would be palliative sedation, which is necessary in this instance to mitigate suffering from significant dyspnea.8
Nausea
The pathophysiology underlying nausea in a dying patient is often multifactorial and can include drugs, organ failure, metabolic disorder, obstruction, constipation, gastroparesis, inflammation, and tumors, to name a few. Nausea is usually treated based on suspected etiology; however, empiric antiemetic therapy has been shown to be equally effective.11,12
Secretions
The “death rattle” refers to the sound that is made when air passes through a dying patient’s pooled secretions within the posterior oropharynx. The rattle is not harmful to the dying patient but is often the most distressing symptom to the family. Proper positioning can facilitate drainage of secretions, but atropine and glycopyrrolate (a quaternary amine that does not cross the blood-brain barrier and therefore does not contribute to terminal delirium) are appropriate drugs in the acute setting to decrease secretions and mitigate noisy respiration.5 Aggressive suctioning should be avoided in the dying patient as comfort of the patient is the goal.
Anxiety, Agitation, and Delirium
Haloperidol has the best data in treating agitation or delirium in this patient population. Droperidol may also be effective, but there is less evidence to support its use. Benzodiazepines can cause paradoxical agitation in elderly patients and should be used as a second-line option with close monitoring of the patient.5,8 If terminal delirium is refractory to initial medications, consult a palliative physician to assist with palliative sedation.
Case Conclusion
You are able to find a quiet room for the patient and his family. You place a nasal cannula for comfort and review the patient’s opioid home regimen as 60 mg extended-release morphine sulfate BID with a rescue dose of 20 mg every four hours for a total oral morphine equivalent of 240 mg that can be converted to 80 mg (3:1 PO:parenteral) in a 24-hour period. Because the patient is not opioid-naive, you give his typical home dose with a 50 percent reduction (10 mg IV) and write for an additional 50 percent of his breakthrough pain dose (3 mg IV) to be given every 30 minutes PRN for severe pain. This dose of opioids will also help manage his dyspnea. For nausea, you select ondansetron 4 mg. Physicians should use an online opioid conversion calculator, such as https://clincalc.com/opioids or https://opioidcalculator.practicalpainmanagement.com, or consult their ED pharmacist when converting oral to IV opioid formulations.
After your interventions, the patient appears much more calm and comfortable. His heart and respiratory rates come down. The patient dies comfortably with family at bedside less than an hour later. They are very appreciative of the care and support provided by the emergency team.
Dr. Vertelney is an emergency medicine resident at the University of California, San Francisco.
 Dr. Garcia is a hospice and palliative medicine fellow at Dell Seton Medical Center at The University of Texas at Austin.
Dr. Garcia is a hospice and palliative medicine fellow at Dell Seton Medical Center at The University of Texas at Austin.
 Dr. Isaacs is an emergency physician at Zuckerberg San Francisco General Hospital; clinical professor of emergency medicine at the University of California, San Francisco; and immediate past Chair of the ACEP Palliative Medicine Section.
Dr. Isaacs is an emergency physician at Zuckerberg San Francisco General Hospital; clinical professor of emergency medicine at the University of California, San Francisco; and immediate past Chair of the ACEP Palliative Medicine Section.
References
- Shreves A, Marcolini E. End of life/palliative care/ethics. Emerg Med Clin North Am. 2014; 32(4):955-974.
- Green E, Ward S, Brierley W, et al. “They shouldn’t be coming to the ED, should they?”: a descriptive service evaluation of why patients with palliative care needs present to the emergency department. Am J Hosp Palliat Care. 2017;34(10):984-990.
- Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010;182(6):563-568.
- Vandyk AD, Harrison MB, Macartney G, et al. Emergency department visits for symptoms experienced by oncology patients: a systematic review. Support Care Cancer. 2012;20(8):1589-1599.
- Lin KJ, Ching A, Edmonds KP, et al. Variable patterns of continuous morphine infusions at end of life. J Palliat Med. 2015;18(9):786-789.
- Fohr SA. The double effect of pain medication: separating myth from reality. J Palliat Med. 1998;1(4):315-328.
- Wang DH. Beyond code status: palliative care begins in the emergency department. Ann Emerg Med. 2017;69(4):437-443.
- Clemens KE, Klaschik E. Symptomatic therapy of dyspnea with strong opioids and its effect on ventilation in palliative care patients. J Pain Symptom Manage. 2007;33(4):473-481.
- Sykes N, Thorns A. The use of opioids and sedatives at the end of life. Lancet Oncol. 2003;4(5):312-318.
- Stephenson J, Davies A. An assessment of aetiology-based guidelines for the management of nausea and vomiting in patients with advanced cancer. Support Care Cancer. 2006;14(4):348-353.
- Davis MP, Hallerberg G, Palliative Medicine Study Group of the Multinational Association of Supportive Care in Cancer. A systematic review of the treatment of nausea and/or vomiting in cancer unrelated to chemotherapy or radiation. J Pain Symptom Manage. 2010;39(4):756-767.
Pages: 1 2 3 4 | Multi-Page




No Responses to “Managing Pain Relief in Palliative Care”