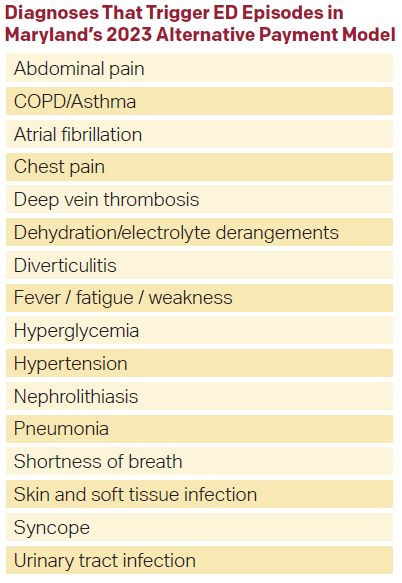
In January 2023, the state of Maryland launched the first-ever government-based emergency medicine alternative payment model. An alternative payment model is a different way of paying for physician services from the usual model: see a patient, send a bill, and get paid, also known as fee-for-service. In the program, Medicare patients who visit a participating emergency department (ED) with specific diagnoses will have their 14-day total cost of care measured across all settings by the state regulatory agency, also known as the Health Services Cost Review Commission (HSCRC). The ED diagnoses chosen for the program include conditions like chest pain, syncope, pneumonia, and others where there are differences between physicians in which patients get admitted, i.e., admissions that seem at times subjective.1 In total, the program includes 535 ED diagnoses. Broad categories of diagnoses in the 2023 model are listed on the related chart. If Medicare patients have any of those diagnosis when they enter a participating ED, they are included in the cost calculations.2 More than 600 emergency department (ED) clinicians in the state are participating in the program.
Explore This Issue
ACEP Now: Vol 42 – No 12 – December 2023Here’s How It Works
Average 14-day Medicare costs of care by diagnoses are measured at the hospital-level and calculated by the HSCRC. This includes the ED visit, hospital admission (should it occur), and any post-acute costs. These costs are compared to 2019 costs, adjusted for inflation, which is also calculated by the HSCRC. If costs are reduced more than 3 percent relative to the baseline, participating physician groups will receive a proportion of the savings. As an example, let’s say 14-day costs for chest pain–one of the included diagnoses—for a physician group were $3,000 on average in 2019. In 2023, that number falls to $2,500 based on ED protocols to increase outpatient management and safely avoid hospital admission. The physician group gets a certain proportion of the $500 savings for each chest pain patient—either 20, 50 percent, or 80 percent. That proportion is determined by the state regulatory agency based on how efficient the group was in 2019, compared to other groups in the state. So, let’s say the group sees 500 chest pain patients in 2023, saves $500 on each, gets 50 percent of the savings back. That means the group gets a payment of $125,000 from the state. Importantly, there are no penalties if costs rise in this model; that is, if the cost goes from $3,000 in 2019 to $3,500 in 2023.
 Nevertheless, the primary way groups will be successful under this model is through implementing evidence-based protocols surrounding hospital admission because that is the primary vector for 14-day total cost of care after an ED visit. Examples include using the HEART score for chest pain admissions or atrial fibrillation discharge pathways.3 Groups also should identify high admitting emergency physicians in their practices who can be coached on using evidence-based decision rules.
Nevertheless, the primary way groups will be successful under this model is through implementing evidence-based protocols surrounding hospital admission because that is the primary vector for 14-day total cost of care after an ED visit. Examples include using the HEART score for chest pain admissions or atrial fibrillation discharge pathways.3 Groups also should identify high admitting emergency physicians in their practices who can be coached on using evidence-based decision rules.
Ground Zero for Payment Models
Maryland is ground zero for payment reform because it has dedicated local mechanisms in place to administer programs through the HSCRC. Since the 1970s, a Centers for Medicare and Medicaid Services (CMS) waiver has allowed all hospital payments in Maryland to be regulated by the state’s HSCRC. This allows HSCRC to be nimble and experiment with new payment models proposed by local stakeholders. In the case of this program, it was designed by ED physicians in a partnership between state clinical leaders through the Maryland ACEP, HSCRC, MedChi (the Maryland physician society), and the Maryland Hospital Association. Additionally, the program is classified as an advanced alternative payment model (AAPM). Thus, participating physicians will also receive a 3.5 percent bonus on all Medicare claims, on top of any shared savings. Participating physicians are also not required to submit data to the Merit-based Incentive Payment System (MIPS) program through CMS, nor be subject to its rewards or penalties.
While the Maryland program is a step in the right direction for ED value-based care, it will likely serve as a temporary program, lasting only a few years. This is because all shared savings programs, like accountable care organizations (ACOs) and others, tend to have a limited shelf life. The basis of shared savings models is reducing costs of care compared to a prior baseline. This cannot occur indefinitely. Ultimately, the only durable long-term alternative payment model is global budgets for emergency physicians, similar to capitation for primary care physicians.. Emergency physician global budgets would be designed to align physician payments directly with population health goals. Maryland would be a great place to test ED physician global budgets because hospitals already receive all-payer global budgets for both inpatient and outpatient services through the state’s Global Budget Revenue (GBR) program through HSCRC. Hospital GBR has been by far the most successful alternative payment in reducing costs.4 Additionally because hospitals are already on GBR, they are already aligned with population health goals.
Here’s how it would work. Imagine an ED has a fixed amount of money to hire emergency physicians to manage care for a population. Under this model, it is unlikely that we would choose to only sit in crowded EDs and deliver care only when available treatment spaces opened. We would move beyond the ED, where our patients could benefit from our skills in helping them decide where to seek care and ensuring continuity after their ED visit. Other elements of an ED physician global budget that would facilitate the move to population health would include additional payments for emergency telehealth to help guide patients to the ideal site of care, follow-up telehealth –or other digital connections—to ensure patients have recovered after their ED visit, and resources for programs that focus on ED frequent users. Other elements could include mandating specific staffing levels to allow for reserve capacity and working to align metrics with hospitals around ED flow, including addressing boarding.
Kaiser Permanente (KP), an integrated delivery system, works through capitation. It has focused efforts on population health through alignment of incentives across their health plan, hospital foundation, and medical group.4 Population-level ED utilization is about one-third lower than the rest of California in adults less younger than 65. For older adults, ED use is similar, but admission rates are one-third lower. KP has a demand management strategy, actively optimizing efficient use of health care resources through their on-call advice line, and access to same or next day outpatient appointments. A central feature is chronic disease management, focusing on treatment in the ED and coordination with outpatient specialists rather than hospital admission. While the KP model is not perfect, it aligns the incentives of acute care with providing the best value for a fixed budget.
Ultimately, how will value-based programs affect the day-to-day role of emergency physicians? That answer depends on whether these models take hold broadly, which is currently unknown, or how emergency medicine is integrated into other value-based care models that focus on primary care, hospitals, and specialists. But what is increasingly certain is that the role of the emergency physician in the health care continuum may change dramatically as these payment models evolve.
 Dr. Leubitz is an innovation fellow at US Acute Care Solutions. He works as an emergency physician at Adventist Shady Grove Hospital in Rockville, MD.
Dr. Leubitz is an innovation fellow at US Acute Care Solutions. He works as an emergency physician at Adventist Shady Grove Hospital in Rockville, MD.
 Dr. Pines is the national director of clinical innovation at US Acute Care Solutions. and a professor of emergency medicine at Drexel University.
Dr. Pines is the national director of clinical innovation at US Acute Care Solutions. and a professor of emergency medicine at Drexel University.
References
- Oskvarek JJ, Zocchi MS, Cai A, et al. Development and internal validation of an emergency department admission intensity measure using data from a national group. Ann Emerg Med. 2023 Sep;82(3):316-325.
- Pines JM, Isserman JA, Szyld D, et al. The effect of physician risk tolerance and the presence of an observation unit on decision making for ED patients with chest pain. Am J Emerg Med. 2010;28:771-9.
- Baugh CW, Clark CL, Wilson JW, et al. Creation and implementation of an outpatient pathway for atrial fibrillation in the emergency department setting: results of an expert panel. Acad Emerg Med. 2018;25:1065-1075.
- Selevan J, Kindermann D, Pines JM, et al. What accountable care organizations can learn from Kaiser Permanente California’s acute care strategy. Popul Health Manag. 2015;18:233-6.
Pages: 1 2 3 4 | Multi-Page





No Responses to “Maryland Implements Value-Based Alternative Payment Model”