For more on the National Hospital Ambulatory Medical Care Survey, see the Nov. 2014 Special Ops column, available at ACEP Now.
Explore This Issue
ACEP Now: Vol 34 – No 01– January 2015The Centers for Disease Control and Prevention provides a wealth of information on emergency medicine in America through the National Hospital Ambulatory Medical Care Survey. The 2011 data report is based on a sampling of 31,084 ED patient care reports from 322 emergency departments. National population census data were used to estimate utilization of ED services by populations. The calendar year 2011 emergency department summary table.
It is critical that emergency physicians and ED leaders understand the data and trends in this report and apply results to local operations. The report, with local community analysis, should be discussed with hospital and community leaders.
The data indicate that the emergency department is an important and valuable element of the health care system. The survey now has 20 years of annual data. In that time, ED visits have grown from 90 million to approximately 136 million, and per capita utilization has grown from 357 visits per 1,000 population to 445 visits per 1,000. Injuries continue to shrink as the cause for an ED visit and now account for about 29 percent of our patients. Those older than 75 are most affected by injuries.
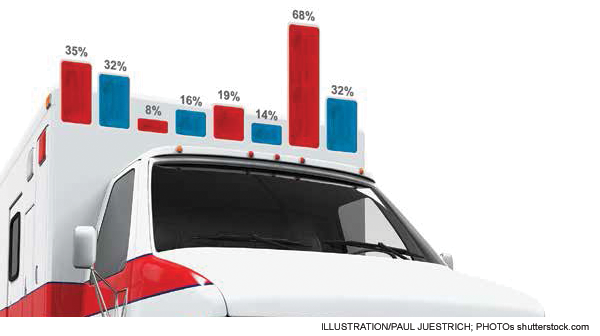
Private insurance or other coverage accounted for about 35 percent of ED visits, Medicaid and the Children’s Health Insurance Program (CHIP) for 32 percent, Medicare for 8 percent, and no insurance for 16 percent. About 16 percent of ED patients arrived by ambulance. A matching number, 16 percent of ED visits, resulted in admission or transfer for admission.
There were 5.3 million ED visits in which a primary mental health issue was noted. About 1.7 million of those visits resulted in hospital admission to a mental health or detoxification unit.
The use of diagnostic testing and treatment continues several trends. More patients are presenting with symptoms that raise issues about a cardiac etiology. Nineteen percent of ED patients had an electrocardiogram performed, and about 14 percent had cardiac enzyme studies. There was a slight decrease in utilization of CT scans but an increasing number of MRIs being performed.
Also, 3.2 percent of ED visits ended with patients leaving before the ED visit was completed, and about 183,000 persons died in the ED or were dead on arrival.
There are hospital-quality indicators related to readmissions to the hospital and revisits to the ED. Emergency physicians must be aware of the baseline level of activity in these metrics. The 2011 data indicate that 6.3 percent of patients admitted through the ED had been discharged from a hospital in the previous seven days, and at least 4 percent of visits were made by patients who had been seen in the same ED in the preceding 72 hours.
There is continuing growth in the percentage of overall hospital admissions presenting through the ED. The 2011 data survey finds that about 22 million admissions occurred through the ED. There were about 35 million hospital discharges, which included newborn infants from hospital delivery units. That means about 63 percent of inpatients were processed through the ED. The Emergency Department Benchmarking Alliance data survey finds an even higher number, with 68 percent of hospital inpatients arriving through the ED. The ED is clearly the “front door of the hospital.”
There is a long-term trend that American EDs are seeing between 2 and 3 percent more visits every year. More patients arrive with medical illnesses rather than injuries. More patients are elderly and arrive by emergency medical services.
The growing number of patients with primary mental health and substance abuse issues represents a serious challenge for emergency physicians.
It is clear that Americans have come to trust the quality of our service and the value for the time and money spent for their ED visits. Emergency physicians should continue to deliver services that provide a reliable and cost-effective system of unscheduled care.
 James J. Augustine, MD, FACEP, is director of clinical operations at EMP in Canton, Ohio; clinical associate professor of Emergency Medicine at Wright State University in Dayton, Ohio; vice president of the Emergency Department Benchmarking Alliance; and on the ACEP Board of Directors.
James J. Augustine, MD, FACEP, is director of clinical operations at EMP in Canton, Ohio; clinical associate professor of Emergency Medicine at Wright State University in Dayton, Ohio; vice president of the Emergency Department Benchmarking Alliance; and on the ACEP Board of Directors.
Pages: 1 2 | Multi-Page






One Response to “National Hospital Ambulatory Medical Care Survey Data Show Increase in Emergency Department Visits”
September 11, 2015
Using Electronic Medical Records to Predict Readmission Risk After Percutaneous Coronary Intervention - ACEP Now[…] characteristics derived from electronic medical records (EMR) can predict the risk of readmission after percutaneous coronary intervention (PCI), a study […]