
Explore This Issue
ACEP Now: Vol 36 – No 03 – March 2017Photo: “New born spinal tap” by Bobjgalindo, licensed underCreative Commons Attribution-ShareAlike 4.0 International License <https://creativecommons.org/licenses/by-sa/4.0/>.
The Case
An 11-day-old female neonate with a chief complaint of jaundice was brought to the emergency department by her father. Other symptoms included spitting up with feeding and tactile fever. The patient’s birth history was significant for a full-term vaginal delivery to a mother who was group B streptococcus (GBS) positive during delivery. The father stated that his daughter had been very “good” since birth, had been very “calm,” and almost never cried. On physical examination, the neonate appeared toxic, listless, and jaundiced and was actively vomiting. The initial workup in the emergency department included urinalysis, complete blood count (CBC), and chest X-ray, all of which were unremarkable except for total bilirubin of 19 mg/dL.
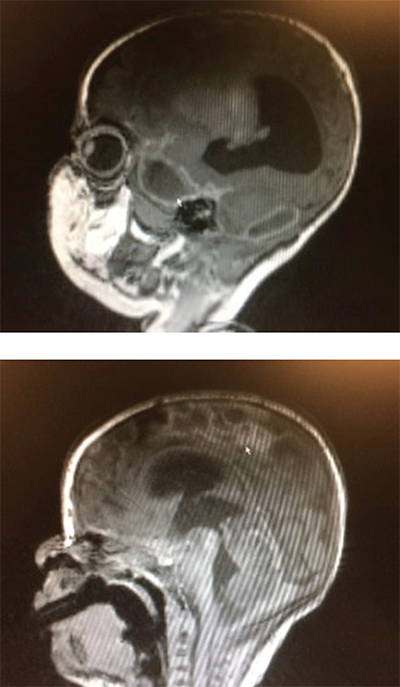
Figure 1 (TOP): Sagittal brain MRI demonstrating a focal area of ischemia (arrow) secondary to meningitis.
Figure 2: Sagittal brain MRI. The ring-encasing lesion (arrow) is demonstrative of subdural empyema in the midbrain secondary to bacterial meningitis.
Photos: Pingching N. Kwan
Given the child’s presentation, age, and birth history, bacterial meningitis was suspected, and a lumbar puncture was suggested. The child’s mother, whom the father was talking to over the phone, initially refused the procedure. However, after extensive discussion about the reasons the procedure was indicated and the low rates of complications associated with the procedure, the child’s mother was convinced, and verbal consent was obtained. The lumbar puncture was performed, and a scant amount (1 mL) of cerebrospinal fluid (CSF), which appeared to be xanthochromic and turbid, was obtained. The child was listless during the procedure. The fluid was sent for analysis and culture, and the child was started on empiric ampicillin and ceftazidime for suspected bacterial meningitis. The child was admitted to the NICU. CSF analysis and culture confirmed the diagnosis of Escherichia coli meningitis. E. coli was sensitive to cephalosporins.
During her hospital course in the NICU, the child subsequently developed persistent seizures and hydrocephalus. A cranial MRI demonstrated ischemic damage to the brain secondary to meningitis (see Figure 1, arrow) as well as a ring enhancing area in the midbrain (see Figure 2, arrow) representing a subdural empyema. The child was treated with five weeks of IV antibiotics. Unfortunately, her neurological prognosis remains poor.
Discussion
Neonatal meningitis is most commonly caused by vertical transmission of GBS (Streptococcus agalactiae) during delivery, implicated in nearly 50 percent of all cases. Other common pathogens include E. coli and Listeria monocytogenes.1 The cumulative incidence of meningitis is highest in the first month of life and is higher in preterm neonates than term neonates.2 Patients may present with difficulty feeding, apnea, bradycardia, hypotension, irritability, or lethargy. Stupor and irritability are common in late-onset meningitis as are neurological complications. A 2015 study demonstrated that central nervous system complications associated with late-onset GBS meningitis, such as hydrocephalus, epilepsy, subdural empyema, and ischemia, may be underestimated.3
Pages: 1 2 3 | Single Page




One Response to “Neonatal Meningitis Diagnosis Difficult Given Subtle Symptoms of Vomiting, Irritability”
March 9, 2023
Daniel MeressaGood diagnosis with good investigation will end up with good treatment and follow-up