In June 2016, the ACEP Board of Directors approved a new clinical policy on the evaluation of adult patients with suspected transient ischemic attack (TIA), which was developed by ACEP’s Clinical Policies Committee. This clinical policy can also be found on ACEP’s website, and has been submitted for inclusion on the National Guideline Clearinghouse website.
Explore This Issue
ACEP Now: Vol 35 – No 11 – November 2016TIA is part of a spectrum that involves ischemia of the central nervous system, with approximately 240,000 cases a year in the United States. Although most TIAs last less than one to two hours, by definition, ‘TIAs have a resolution of symptoms within 24 hours without evidence of an acute infarction on imaging. Since approximately 15 percent of all ischemic strokes are preceded by a TIA, timely evaluation for high-risk conditions, such as carotid stenosis and atrial fibrillation, is important.
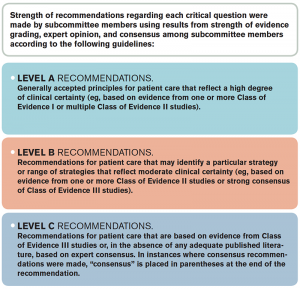
Based on the feedback from the ACEP membership, the committee focused on four clinical questions about the evaluation of TIA in the emergency department. A systematic review of the evidence was conducted, and the committee made recommendations (A, B, or C) based on the strength of evidence (see Table 1). This clinical policy received input and comments from emergency physicians, neurologists, and members of the American Heart Association/American Stroke Association during the 60-day open-comment period. These responses were used to refine and enhance this clinical policy.
If non-contrast brain MRI is not readily available, it’s reasonable for physicians to obtain a non-contrast head CT as part of the initial TIA workup to identify TIA mimics (eg, intracranial hemorrhage, mass lesion). However, non-contrast head CT should not be used to identify patients at high, short-term risk for stroke.
Critical Questions and Recommendations
Question 1. In adult patients with suspected TIA, are there clinical decision rules that can identify patients at very low short-term risk for stroke who can be safely discharged from the emergency department?
Patient Management Recommendations
- Level A: None specified.
- Level B: In adult patients with suspected TIA, do not rely on current existing risk stratification instruments (eg, ABCD2 score) to identify TIA patients who can be safely discharged from the emergency department.
- Level C: None specified.
Question 2. In adult patients with suspected TIA, what imaging can be safely delayed from the initial ED workup?
Patient Management Recommendations
- Level A: None specified.
- Level B: None specified.
- Level C: (1) The safety of delaying neuroimaging from the initial ED workup is unknown. If non-contrast brain MRI is not readily available, it’s reasonable for physicians to obtain a non-contrast head CT as part of the initial TIA workup to identify TIA mimics (eg, intracranial hemorrhage, mass lesion). However, non-contrast head CT should not be used to identify patients at high, short-term risk for stroke. (2) When feasible, physicians should obtain MRI with diffusion-weighted imaging to identify patients at high short-term risk for stroke. (3) When feasible, physicians should obtain cervical vascular imaging (eg, carotid ultrasonography, CT angiography [CTA], or magnetic resonance angiography [MRA]) to identify patients at high short-term risk for stroke.
Question 3. In adult patients with suspected TIA, is carotid ultrasonography as accurate as neck CTA or MRA in identifying severe carotid stenosis?
Patient Management Recommendations
- Level A: None specified.
- Level B: None specified.
- Level C: In adult patients with suspected TIA, carotid ultrasonography may be used to exclude severe carotid stenosis because it has an accuracy similar to that of MRA or CTA.
Question 4. In adult patients with suspected TIA, can a rapid ED-based diagnostic protocol safely identify patients at short-term risk for stroke?
Patient Management Recommendations
- Level A: None specified.
- Level B: In adult patients with suspected TIA without high-risk conditions, a rapid ED-based diagnostic protocol may be used to evaluate patients at short-term risk for stroke. (High-risk conditions include abnormal initial head CT result [if obtained], suspected embolic source [presence of atrial fibrillation, cardiomyopathy, or valvulopathy], known carotid stenosis, previous large stroke, and crescendo TIA.)
- Level C: None specified.
Because of the high risk of stroke after a TIA, timely diagnostic testing for modifiable risk factors is important. This can be done in a number of ways, including an ED-based protocol (eg, ED observation) and should include neurovascular imaging.
While there are a number of risk stratification instruments for TIA, none are currently sufficient in identifying patients who are at low short-term risk for stroke and who can be safely discharged from the ED. More research is needed to develop better risk-stratification instruments as well as identifying which diagnostics tests should be performed during the ED visit versus as an outpatient.
Dr. Lo is an associate professor of emergency medicine at Eastern Virginia Medical School, Norfolk, Virginia, and medical director of the department of emergency medicine at Sentara Norfolk General Hospital, Norfolk, Virginia.
Pages: 1 2 | Multi-Page





2 Responses to “New ACEP Clinical Policy on Transient Ischemic Attack”
November 21, 2016
Jonathan S Fried MDNot much help, why publish a new clinical policy, if it has so little to offer?
November 28, 2016
Kurt Kaczander, DOAgreed. Nebulous recommendations that don’t aid in our decision making..