
Recommendations cover staffing, education, equipment, procedures, follow-up tips, and performance improvement measures for geriatric emergency care
Explore This Issue
ACEP Now: Vol 33 – No 03 – March 2014The Geriatric Emergency Department Guidelines (GED) (www.acep.org/geriEDguidelines) were the collaborative effort of members of ACEP, American Geriatrics Society (AGS), Emergency Nurses Association (ENA), and Society for Academic Emergency Medicine (SAEM). The strength of this document is evidenced by the approval of each organization’s Board of Directors and copyright of the material in 2013. ACEP states, “the purpose of the Geriatric Emergency Department Guidelines is to provide a standardized set of guidelines that can effectively improve the care of the geriatric population and are feasible to implement in the ED. The guidelines create a template for staffing, equipment, education, policies and procedures, follow-up care, and performance improvement measures.”
These guidelines represent recommendations for geriatric emergency care. They are not a mandate for every ED to develop a GED or a list of recommendations requiring 100 percent compliance.
The authors, practicing emergency physicians, as well as emergency nurses and geriatricians, wrote the document for local ED leaders to drive quality geriatric emergency care within their institutions. We anticipate many questions related to these recommendations. This introduction is meant to help ACEP Now readers understand these new recommendations. Specifically, we hope to inform readers about:
- The historical context of geriatrics and emergency medicine
- Why these GED Guidelines are being released now
- How the GED Guidelines were derived
- What constitutes the GED Guidelines
- The present and future plans for the GED Guidelines
Geriatrics and Emergency Medicine—Historical Context
While a constellation of factors precipitated the development of a pediatric emergency medicine infrastructure, the demographic imperative of a rapidly aging baby-boomer society was slower to rouse change in adult emergency medicine. In the 1990s, The John A. Hartford Foundation, led by Donna Regenstrief, decided to focus on improving geriatric health care outcomes at this time. The Hartford Foundation recognized the cross disciplinary role of emergency medicine and approached the University Association of Emergency Medicine (UAEM), the precursor of SAEM, with a challenge to develop a body of expertise in geriatric emergency medical education, research, clinical operations, and policy-making. Art Sanders, MD, the UAEM president, received a small pilot grant from the Hartford Foundation in 1991 and formed the first Geriatric Emergency Medicine Task Force. This task force produced a series of original research manuscripts, essays, and editorials that filled the July 1992 issue of Annals of Emergency Medicine. These works described the current state of affairs for geriatric emergency care while outlining an agenda for future research and educational initiatives. The energy and productivity of this first task force led to a larger grant from the Hartford Foundation in 1993, and that ultimately led to the first textbook (1996’s Emergency Care of the Elder Person, edited by Dr. Sanders), as well as multiple research projects that further defined the epidemiology of geriatric syndromes (falls, delirium, dementia, polypharmacy) in the ED.
Why the Guidelines Are Being Released Now
In 2000, the Geriatric Interest Group was born at SAEM with Chair Lowell Gerson, PhD. By 2011, the group’s accomplishments under leaders Manish Shah, MD, FACEP; Scott Wilber, MD, FACEP; and Ula Hwang, MD, FACEP, led to the transformation of the interest group into the Academy of Geriatric Emergency Medicine (AGEM). The ACEP Board of Directors approved the formation of the Geriatric Section in 2003 after a strong campaign from Jim Espinosa, MD; Kirk Jensen, MD, FACEP; and Marilyn Bromley, RN. Under the leadership of Mark Rosenberg, DO, FACEP, the ACEP Geriatric Section’s membership rapidly grew. These geriatric emergency medicine groups continued to expand the peer reviewed and mass media publication portfolio for optimal older adult acute care. For example, Bob Fitzgerald, MD, FACEP, published the ACEP White Paper “The Future of Geriatric Care in Our Nation’s Emergency Departments” in 2008. Teresita Hogan, MD, FACEP, worked with the American Medical Association, ACEP, SAEM, American Geriatrics Society, Council of Emergency Medicine Residency Directors, Emergency Medicine Residents’ Association, and multiple other stakeholders to develop geriatric core competencies for every emergency medicine resident in 2010. Emergency medicine needed a structured document containing best-practice recommendations from geriatric emergency health care providers, researchers, and advocates. With the support of then ACEP President David Seaberg, MD, FACEP, the process of developing such a document began in early 2011.
The geriatric ED patient represents the “canary in the coal mine” for our health care system. If we can successfully navigate the diagnostic, therapeutic, disposition, and financial challenges that this potentially vulnerable population presents, then all age groups will benefit.
How the GED Guidelines Were Derived
In 2011, Dr. Rosenberg then chair of the ACEP Geriatric Section, organized a Geriatric ED Steering Committee. The goal of the steering committee was to establish standards by which to develop and operate GEDs. The committee was composed of members of the ACEP Geriatric Section and AGEM. The committee also included representatives from AGS and ENA. Work on the guidelines progressed via a series of teleconferences during 2011 and 2012. The 14 GED Guidelines coauthors split into two working groups: “structural and staffing” and “clinical/operational.” Each group reviewed the literature and provided best-evidence recommendations for essential geriatric emergency care. The entire membership of AGEM and the ACEP Geriatric Section formally reviewed and approved the GED Guideline recommendations in October 2012. Between October 2013 and February 2014, Boards of Directors for ACEP, SAEM, AGS, and ENA officially approved the guidelines.
What Constitutes the GED Guidelines? What They Are and What They Are Not
Most health care systems will lack the financial resources, staffing levels, or patient volumes for stand-alone GEDs to be feasible. Instead, these guidelines provide a basis from which EDs can consider ways to improve care for older adults. In 2007, when the first GED paper described the special care needs of geriatric patients, no GEDs existed in the United States. Currently, more than 40 self-designated “Geriatric EDs” or “Senior ERs” exist, and these guidelines provide concrete, feasible, and measurable recommendations to consider should an ED declare itself as having a GED. We cannot overemphasize that the GED Guidelines are not a mandate that every geriatric-friendly ED develop and sustain. Every ED that provides emergency care for geriatric adults, however, should be aware of these guidelines, the rationale for the recommendations, and the resources available to transition from theory to implementation.
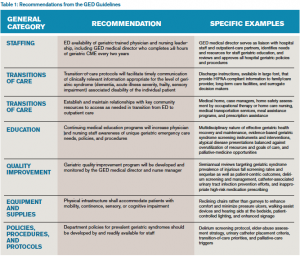
The GED Guidelines consist of 40 specific recommendations in six general categories: staffing, transitions of care, education, quality improvement, equipment/supplies, and policies/procedures/protocols. Staffing includes recommendations for the medical director and nurse manager and accessibility to specialist ancillary services. Transitions of care include discharge processes and large-font instructions, as well as appropriate collaboration with home health services and home safety assessments. Nurse and clinical provider education focuses on contemporary, research-based geriatric-specific material. The quality improvement recommendations provide an exemplar spreadsheet of pertinent and prevalent geriatric emergency care indicators to monitor, including the prevalence of injurious falls and documentation of fall risk assessment. The equipment and supplies section describes potential physical structure enhancements like the use of reclining chairs and pressure redistributing foam mattresses to improve comfort and reduce the incidence of pressure ulcers. Finally, a variety of policies, procedures, and protocols are provided to facilitate screening older adults to identify the subset who are at increased risk for post-ED adverse outcomes, as well as validated, ED feasible screening instruments for geriatric syndromes such as delirium, polypharmacy, falls, and dementia. See Table 1 for more details about specific GED recommendations that should provide further clarity about the content of the GED Guidelines.
The Present and Future Plans for the GED Guidelines
These guidelines represent a two-year effort from multiple organizations and individuals committed to optimizing the emergency care delivery model for geriatrics. We believe that the geriatric ED patient represents the “canary in the coal mine” for our health care system. If we can successfully navigate the diagnostic, therapeutic, disposition, and financial challenges that this potentially vulnerable population presents to 21st-century medicine, then all age groups will benefit from a reliable, available, compassionate, and efficient emergency care system. We fully recognize that the GED Guidelines are a beginning and not an end. The authors have defined a plan that includes dissemination, implementation, adaptation, and refinement. The empiric basis for the recommendations rests upon minimal research evidence. To move forward, geriatric emergency medicine needs sustainable funding opportunities to: 1) enhance the evidentiary basis of these protocols; 2) determine if following these recommendations does, in fact, improve the process and quality of care delivered; 3) determine if the recommendations improve health care outcomes for older adults and their caregivers; and 4) support the growth and evolution of future geriatric emergency medicine leaders.
One immediate next step is to prioritize, in a systematic and transparent way, the 40 recommendations into essential and nonessential domains so hospital administrators, payers, and research funders can develop a systematic approach to local implementation. For example, routinely screening for delirium using validated instruments has profound implications on ED disposition and management decisions as opposed to infrastructural changes to lighting, floor material, and wall colors. The prioritization process will assess the relative potential benefits and potential harms associated with each recommendation in providing a weighted list from most to least important. Another step is to raise GED Guidelines awareness among emergency medicine clinicians, hospital administrators, patient advocacy leaders, and patients. The GED Guidelines group is also developing a “Geriatric Emergency Department Boot Camp” program, in which geriatric emergency medicine leaders will bring the recommendations to those interested, including a toolbox of resources, pragmatic examples from their own institutions, and mentorship. The benefit of the boot camp concept is that hospitals interested in “geriatricizing” their ED need not travel to learn more about these implementation recommendations, and essential interdisciplinary members (i.e., social workers, case managers, pharmacists, hospital administrators, and payers) can also participate via this boot camp idea. The intent is for participants in the boot camps to devise local and regional needs-based quality-improvement projects, which the boot camp faculty can assist; one-year outcomes will be assessed. The boot camp concept also provides a tangible test tube to evaluate the feasibility, acceptability, and barriers to implementing existing GED Guideline recommendations.
The public release of the GED Guidelines represents an effort to transform emergency care for older adults. The unique health care needs of our aging population will challenge our health care system in and beyond the ED. For all hospitals, geriatric-only EDs will not be a mandate nor are they necessary. However, geriatricizing our EDs to provide optimal care for older adults will be a necessity.
Dr. Carpenter is chair of the ACEP Geriatric Section.
Dr. Hwang is president of the SAEM Academy for Geriatric Emergency Medicine.
Dr. Rosenberg is immediate past chair of the ACEP Geriatric Section and is on the board of directors of the SAEM Academy for Geriatric Emergency Medicine.
Pages: 1 2 3 | Multi-Page





2 Responses to “New Guidelines Enhance Care Standards for Elderly Patients in the ED”
November 23, 2014
Aslaner: Geriartrik Acil Servis Kılavuzu | Acilci.Net: Acil Tıp Eğitimi için EKG, Kılavuz, Video ve Sunumlar[…] https://www.acepnow.com/article/new-guidelines-enhance-care-standards-elderly-patients-ed/. […]
August 13, 2015
Elderly Patients Want to Be in Control of Their Health Information - ACEP Now[…] Elderly patients may be willing to let family members access their medical records and make decisions on their behalf, but they also want to retain granular control of their health information, a study suggests. […]