“Whoop, whoop, whoop!” The EMS radio alerts the ED staff to an incoming patient. Minutes later arrives a patient who has a 33 percent chance of being moved to an inpatient bed in about five hours, a 5 percent chance of being moved to the ICU in about three hours, and a chance of being moved onto a medical helicopter or onto a medical examiner’s table.
Explore This Issue
ACEP Now: Vol 38 – No 05 – May 2019For those emergency physicians working in medical centers that specialize in trauma, burns, acute cardiac intervention, and comprehensive stroke care, those ambulance patients represent the vast majority of patients who pay for such specialty programs and services. For those who don’t like ambulance patients, the future is arriving faster than a medic unit running lights and sirens.
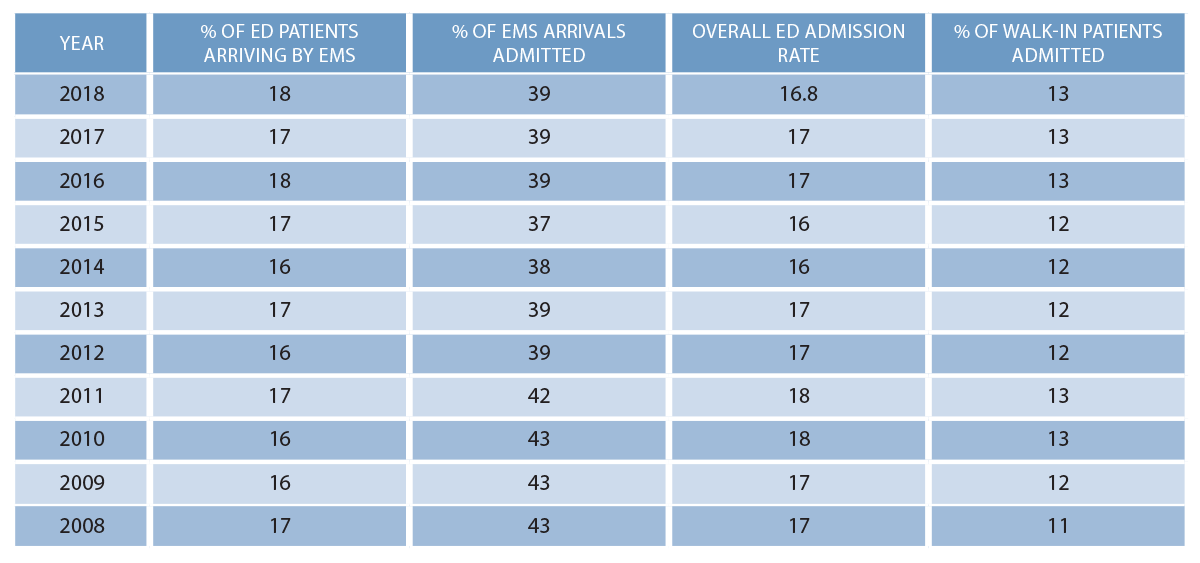
Studying the Emergency Department Benchmarking Alliance (EDBA) data over the last 10 years, we find that EMS arrivals and admission rates are predictable, and ambulance patients continue to represent higher acuity than those arriving in a private automobile or other conveyance. Table 1 demonstrates that about 39 percent of EMS-arriving patients are admitted. Patients arriving by other means have a significantly lower admission rate of about 12.5 percent.
CMS Launches New Payment Model
On Feb. 14, 2019, the Centers for Medicare and Medicaid Services (CMS) announced a new payment model for unscheduled care responders that pays for care that does not include transportation to the hospital.1 The proposed Emergency Triage, Treat, and Transport (ET3) Model will pay for care provided out of hospital, either in person or through telehealth processes. It also pays EMS responders to transport patients by ambulance to alternative out-of-hospital care sites, including urgent care or a primary care provider.
The model’s announced goal is to end the incentives for first responders to transport patients to the emergency department. The program is being introduced by the Center for Medicare and Medicaid Innovation as a method to improve the quality of care for unscheduled health events and is targeted to save the health care system $1 billion in avoidable ED costs. CMS believes 19 percent of Medicare fee-for-service beneficiaries could be treated at home or in another cheaper facility for their emergency needs. CMS also hopes Medicaid managed care plans and private payers will take an interest in the voluntary model.
Program rules have yet to be written, and it may take six or more months until applicants for the model are recruited. However, EMS providers selected to participate will have options in how they wish to structure the on-site element. Options will include a telehealth-heavy model in which a physician or advanced practice provider provides care on-site or remotely. The fact sheet says the demonstration will last five years.
The bottom line? There are evolving models of care that feature alternate providers paid to deliver a variety of services outside of the traditional model of emergency care delivered in the emergency department.
Pages: 1 2 3 | Single Page





No Responses to “New Out-Of-Hospital Care Models Could Affect Your Emergency Dept”