The Case
A 35-year-old man presents to the emergency department after falling off his bicycle. After basic trauma evaluation, a mildly displaced fracture is noted on the distal third of the clavicle. The patient has moderate to severe pain in that area after intravenous opioid and oral NSAID therapy. A multimodal approach to pain control with an ultrasound-guided superior cervical plexus (SCP) block is offered to the patient.
Explore This Issue
ACEP Now: Vol 33 – No 11 – November 2014Unlike other common nerve blocks, the SCP block does not target an individual nerve but instead targets the fascial plane containing the SCP.
Introduction
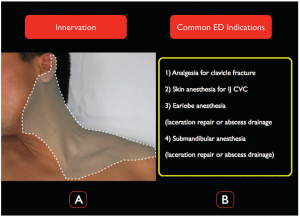
The ultrasound-guided SCP block provides anesthesia to the superficial structures of the neck and shoulder, much of the earlobe, and the superior portion of the shoulder (Figure 1A). In the ED, the SCP block is used for clavicle fracture analgesia, as an alternative to local anesthetic infiltration for internal jugular central venous cannulation (CVC), or abscess drainage/laceration repair on the neck or earlobe (Figure 1B). For clinicians already familiar with performing ultrasound-guided internal jugular CVCs, sonographic localization of the target plane for an SCP block is easily accomplished with a stepwise approach to anterior neck anatomy. Once the emergency physician is comfortable with ultrasonographic needle tip visualization, the SCP block can be rapidly integrated into the clinical armamentarium.
(click for larger image)
Figure 1.
A) The distribution of the SCP block. Note that the innervation extends down to the T2 level and to the cape of the shoulder. B) Common emergency medicine indications for the SCP block.
Anatomy
The superior cervical plexus originates from the C1–C4 anterior rami and emerges from the posterior border of the sternocleidomastoid (SCM) muscle at the level of the superior pole of the thyroid cartilage. The SCP is composed of four distinct nerves: greater auricular (C2, C3), lesser occipital (C2), transverse cervical (C2, C3), and suprascapular (C3, C4). Together, these nerves provide sensory innervation to a large anatomic area including the skin and superficial structures of the neck, the submandibular area, the area overlying the clavicle and upper chest, and portions of the ear and the superior “cape” of the shoulder (Figure 1). Unlike other common nerve blocks, the SCP block does not target an individual nerve but instead targets the fascial plane containing the SCP. Thus, the components of the plexus are not visualized as individual nerves, but instead appear as a poorly defined grouping of hyperechoic structures not readily distinguishable from the surrounding connective tissue. The goal of the block is to place anesthetic in the fascial plane just underneath the belly of the SCM at the C4 level where the SCP emerges along its posterolateral border.
The Procedure
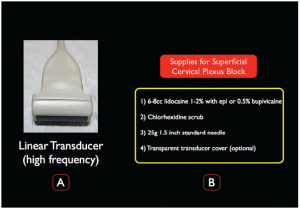
Sterile Preparation. The skin should be prepared with antiseptic solution, and a high-frequency linear (15-6 MHz) ultrasound probe should be disinfected with quaternary ammonia cleaning wipes prior to the procedure. The probe-transducing surface should be covered with a sterile adhesive dressing; a full probe cover is not necessary (Figure 2).
(click for larger image)
Figure 2.
A) A high-frequency linear transducer is ideal for the ultrasound-guided SCP block. B) Supplies needed for the SCP block.
Survey Scan. Place the patient in lateral decubitus position, with the affected side facing up. The ultrasound system should be located contralateral to the affected side, allowing the clinician to comfortably view the screen and the site of injection. Place a high-frequency linear transducer (15-6 MHz) in a transverse plane on the anterior neck at the level of the thyroid cartilage (probe marker pointing medially toward the thyroid). Clinicians who perform ultrasound-guided CVC should be familiar with the sonoanatomy at this level and be able to visualize the internal jugular vein, carotid artery, thyroid, and sternocleidomastoid muscle (Figure 3A). From this familiar position, the probe should be moved cephalad to the C4 level (the superior pole of the thyroid cartilage) and then laterally until the SCM muscle tapers to a beak (Figure 3B). The SCP is located just under the SCM and will be noted as a hyperechoic structure below the SCM and just above the levator scapulae muscle (LSM). Visualization of the interscalene groove or components of the brachial plexus indicates a low position; at the target C4 level, scalene muscles are typically quite small, deep, or not visualized (Figure 3B).
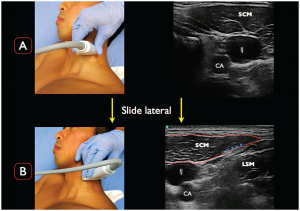
(click for larger image)
Figure 3.
A) Place the transducer in a transverse orientation to the neck at the superior portion of the thyroid cartilage. Note the classic ultrasonographic landmarks; CA= carotid artery; IJ= internal jugular vein; SCM= sternocleidomastoid muscle. B) At the level of the superior portion of the thyroid cartilage, slowly slide the transducer laterally. Note the tapering of the SCM muscle and the LSM just below. The superior cervical plexus (SCP denoted by the blue arrowheads) is the group of hyperechoic structures between the SCM muscle and LSM.
Other commonly used landmarks to ensure the correct cervical level of the SCP block include the midpoint of the SCM from the mastoid to its insertion on the clavicle and the point where the external jugular crosses the posterolateral border of the SCM.
Needle Insertion and Injection. The patient should be placed on continuous cardiac monitoring. Attach a 10 cc syringe filled with 6–8 cc of local anesthetic (eg, bupivacaine 0.5% or lidocaine 1%) to a 25 g 1.5″ needle. After the transducer is placed in a transverse position over the anterior neck, we recommend using color Doppler to confirm the lack of aberrant vasculature. An in-plane posterior approach (lateral to medial) will allow the clinician to clearly visualize the needle during the entire nerve block. The goal is to guide the needle tip just under the tapering posterolateral edge of the SCM to the fascial layer between the SCM and LSM (Figure 4). Gentle aliquots of anesthetic should be placed in this location, ensuring anechoic spread of fluid on the ultrasound screen. Common errors include nonvisualized anesthetic spread and/or placing the needle tip in either the SCM or levator scapulae muscle belly.
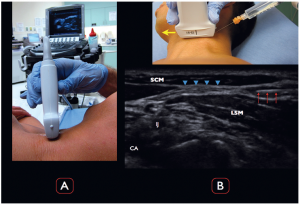
(click for larger image)
Figure 4.
A) The ultrasound screen is contralateral to the affected extremity, with a clear view of the screen for the clinician. B) The needle and needle tip (red arrows) are visualized clearly entering from the lateral aspect of the ultrasound image. Note that the ultrasound transducer directional marker is medial (yellow arrow).
Anechoic anesthetic is being placed between the SCM muscle and LSM, with clear visualization of the needle tip as well as the SCP (blue arrowheads).
Potential Complications. As with all ultrasound-guided nerve blocks, systemic toxicity from inadvertent vascular injection and peripheral nerve injury should always be considered. Specifically for the ultrasound-guided SCP block, if the provider chooses a level too low (C6) or too deep (beneath the prevertebral fascia), phrenic nerve, recurrent laryngeal nerve, deep cervical plexus, or brachial plexus block can occur. Also, a transient Horner’s syndrome can occur if the anesthetic travels deep in the prevertebral fascial plane and reaches the cervical sympathetic chain. Even though uncommon, understanding possible unwanted side effects is imperative for any clinician performing the SCP block (or any procedure).
Dr. Nagdev is director of emergency ultrasound at Highland General Hospital in Oakland, California.
Dr. Herring is an attending physician at Highland General Hospital.
References
- Herring AA, Stone MB, Frenkel O, Chipman A, Nagdev AD. The ultrasound-guided superficial cervical plexus block for anesthesia and analgesia in emergency care settings. Am J Emerg Med. 2012;30:1263-7.
- Shteif M, Lesmes D, Hartman G, Ruffino S, Laster Z. The use of the superficial cervical plexus block in the drainage of submandibular and submental abscesses—an alternative for general anesthesia. J Oral Maxillofac Surg. 2008;66:2642-5.
- Çiftci T, Daskaya H, Yıldırım MB, Söylemez H. A minimally painful, comfortable, and safe technique for hemodialysis catheter placement in children: superficial cervical plexus block. Hemodial Int. 2014;18:700-4.
Pages: 1 2 3 | Multi-Page





One Response to “Pain Control Using Ultrasound-Guided Superficial Cervical Plexus Block”
October 19, 2021
Hazel McArdleCan ultrasound be used for scalene tight muscles