https://www.acepnow.com/wp-content/uploads/2016/05/ACEP_0516_pg20b-e1479151000600.png
Explore This Issue
ACEP Now: Vol 35 – No 11 – November 2016You simply have to know to assess the two questions when examining the patient during your encounter. Then you can pull out your PV card, and voilà, your afebrile well-appearing patient with palpable purpura very likely has autoimmune vasculitis.
Most of the Free Open Access Medical Education (FOAM) that emergency physicians consume comes in forms that you wouldn’t turn to during a shift. Podcasts and blogs are great, but they don’t lend themselves well as on-the-fly references. However, there are some forms of FOAM that you can and should utilize during shifts, and on a recent episode of FOAMcast, we covered some of our favorites. Among the most widely used “just in time” resources for FOAM are the Paucis Verbis (PV) cards published by the blog Academic Life in Emergency Medicine.
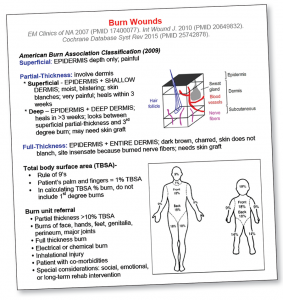
(click for larger image)
This card was updated by Dr. Christian Rose (UCSF-SFGH) to reflect current evidence that topical antibiotics and honey are IN, while silver sulfadiazine is OUT for partial-thickness burns.
www.aliem.com
Currently, there are more than 150 PV cards available in many forms, including individual PDFs that can be saved ad hoc on any device or, if you like to be more organized, in one of several apps in your phone or computer (Evernote, AgileMD, or even a Dropbox folder). We used to recommend saving lots of these on your personal device, but with the ubiquity of the Internet, sometimes we find it is easier to Google the cards when you need them. The topics covered in the PV card series include an impressive range, such as cardiology, hematology, toxicology, and many more.
Among our most favorite PV cards of all time (yes, we have favorite PV cards; we are considering therapy) is “An Approach to Rashes.” The card (actually it’s three pages) is based on a popular article published in The Journal of Emergency Medicine from 2010 by Heather Murphy-Lavoie, MD, and Tracy Leigh LeGros, MD, PhD. The card has a succinct set of definitions of rash descriptors (nodule versus plaque, etc.) and some high-yield reminders (eg, the differential diagnosis of an acute rash co-presenting with hypotension, meningococcemia, toxic shock syndrome, Rocky Mountain spotted fever, toxic epidermal necrolysis, and Stevens-Johnson). Most useful are the four flow charts that provide an excellent framework for rashes that are important to identify in the ED setting.
Undaunted by the fact that FOAMcast is an audio program with absolutely no visual component other than our companion website, we decided to tackle one of the four charts and dedicate an entire show to it. We’re almost positive we are the first people to have ever published an entire podcast about petechiae and purpura. Yeah, we’re kind of proud that we pulled it off.
So if we could do a podcast about rashes without the help of visual aids, then why not try to do our column the same way? Well, here goes.
No Visual Needed
The dermatologists remind us that purpura is the umbrella term for purple discoloration of the skin due to extravasated blood. These lesions don’t blanch. Petechiae are the small ones (less than 3 mm), while ecchymosis are the larger ones (greater than 5 mm.) With that in mind, the purpura flowchart only asks two questions: 1) Is the patient toxic/febrile? 2) Are the lesions palpable or non-palpable? This means that when it comes to pupura, there are only four conditions total: a toxic-appearing/febrile patient with either palpable (1) or non-palpable lesions (2) or a non-toxic-appearing/afebrile patient with either palpable (3) or non-palpable lesions (4). That’s it. The best part is you really don’t have to memorize the differential diagnosis of these four conditions. You simply have to know to assess the two questions when examining the patient during your encounter. Then you can pull out your PV card, and voilà, your afebrile well-appearing patient with palpable purpura very likely has autoimmune vasculitis.
We chose this particular example because the differential diagnosis for that branch of the decision tree conveniently has only one entry. What if that same patient had non-palpable purpura? The only possibility is idiopathic thrombocytopenic purpura (ITP). That means that if you have an overall well-appearing patient with non-blanching purple spots, you know it’s either autoimmune vasculitis or ITP. Now all you would need to do is touch the rash to decide which one it is. If you could feel the lesions, it would be ITP—not bad! The febrile/toxic branches have a few more options for the differential diagnosis, which is why you’ll want to have the PV card handy. The card also has similarly useful flowcharts for maculopapular, erythematous, and vesiculobullous rashes. The major branch points in these decision trees focus, again, on the sick versus not-sick distinction, as well location and distribution of the lesions and the presence or absence of Nikolsky sign. With just those few questions in mind, you can easily delineate an impressive number of rashes.
For more PV cards, check out ALIEM.com, and as always, you can download our recent episodes at FOAMcast.org or on iTunes. In addition to our show on “just in time” FOAMed resources, we’ve recently recorded shows covering news on intracranial hemorrhage management (spoiler: aggressive blood pressure control seems to be unnecessary; also transfusing platelets for spontaneous intracranial hemorrhage might be a bad thing after all), an entire show on the pericardium, and a show covering the various types of altitude-associated illnesses.
 Dr. Faust is a senior emergency-medicine resident at Mount Sinai Hospital in New York. He tweets about #FOAMed and classical music @jeremyfaust.
Dr. Faust is a senior emergency-medicine resident at Mount Sinai Hospital in New York. He tweets about #FOAMed and classical music @jeremyfaust.
 Dr. Westafer is an attending physician and research fellow at Baystate Medical Center, clinical instructor at the University of Massachusetts Medical School in Worcester, and co-host of FOAMcast.
Dr. Westafer is an attending physician and research fellow at Baystate Medical Center, clinical instructor at the University of Massachusetts Medical School in Worcester, and co-host of FOAMcast.
Pages: 1 2 3 | Multi-Page





No Responses to “Paucis Verbis Cards Can Help Determine Diagnosis for Petechiae, Purpura Rashes”