What is fear? These are the opening words of the podcast “The Undifferentiated Sick Infant,” which can be found in the Pediatric Emergency Playbook developed by Tim Horeczko, MD, MSCR, FACEP, the mastermind behind a fantastic new pediatric emergency medicine (PEM) resource.
Explore This Issue
ACEP Now: Vol 35 – No 02 – February 2016No stranger to emergency medicine, even prior to medical school, Dr. Horeczko worked his way through school as a clerk and EMT in a local emergency department. This is where his interest in medicine was born, and after achieving his bachelor’s degree at the University of California (UC) at Berkeley, he attended UC Davis for medical school. He did his residency in emergency medicine, fellowship in PEM, and graduate studies at Harbor–UCLA, where he is now faculty.
Launched in September 2015, Pediatric Emergency Playbook is a monthly podcast addressing some of the current controversies in PEM, including use of intranasal medications, the undifferentiated sick child, and status epilepticus. When compared with some other educational tools, the podcast has the advantage of being available on the go. “The beauty of a podcast is that I can be with you in the car or at the gym or out for a run,” said Dr. Horeczko.
Even though it is relatively new to the scene, Pediatric Emergency Playbook has enjoyed numerous successes already. There are listeners in more than 60 countries, and it was named to the Top 10 Podcasts for medicine in iTunes’ “New and Noteworthy” section. Dr. Horeczko’s goal with this endeavor is to help provide physicians caring for sick children with not only the evidence and practice styles but also some experience. “My goal is to demystify pediatric care and add value to our specialty,” he said. “I try to serve the audience by not just talking about the absolutes in medicine, the ‘yesses’ and the ‘nos,’ including the ‘maybes’ and also the ‘whys.’ It’s about getting at the subtleties and the nuances of what we do. Using the three levels of knowledge—the theoretical, the technical, and the practical—we are able to use our experiences to help teach others.”
Dr. Horeczko gets the inspiration for his podcasts from the problems those physicians caring for sick and injured children face and struggle with every day. He uses his format of presenting a vignette, discussing the evidence behind the problem, putting his own experience to use with some treatment options, and fleshing out some of the controversies involved to help listeners work their way through a common clinical problem.
We have all been there: evaluating the child that presents to our department and is sick—really sick. It may be the 7-day-old with breathing problems or the 5-year-old with vomiting and fever, with every patient bringing their own broad differential and varying approach. In that instant when we start our resuscitation or evaluation, we often remember the words or advice given to us by a mentor or colleague, helping us learn and treat based on their experiences—sometimes successes and sometimes not. That is Dr. Horeczko’s goal with the Playbook: to give pearls and advice on some common (and not so common) pediatric presentations that he has gleaned along the way in an effort to help others.
He starts with Adam, the 7-day-old with breathing problems. The differential diagnosis for such a complaint in this age group is vast, and the first question we often ask ourselves is, is the patient sick? We spend our time teaching students, residents, and fellows the difference between sick and not sick. The Playbook provides some rapid-assessment tools, using both visual graphics (see Figures 1 and 2) and verbal mnemonics to help easily distinguish between sick and not sick. For example, using the mnemonic “TICLS” can help you quickly assess a pediatric patient with undifferentiated illness in a matter of seconds and can give you valuable information:
T = Tone
I = Interactiveness
C = Consolability
L = Look/gaze
S = Speech/cry
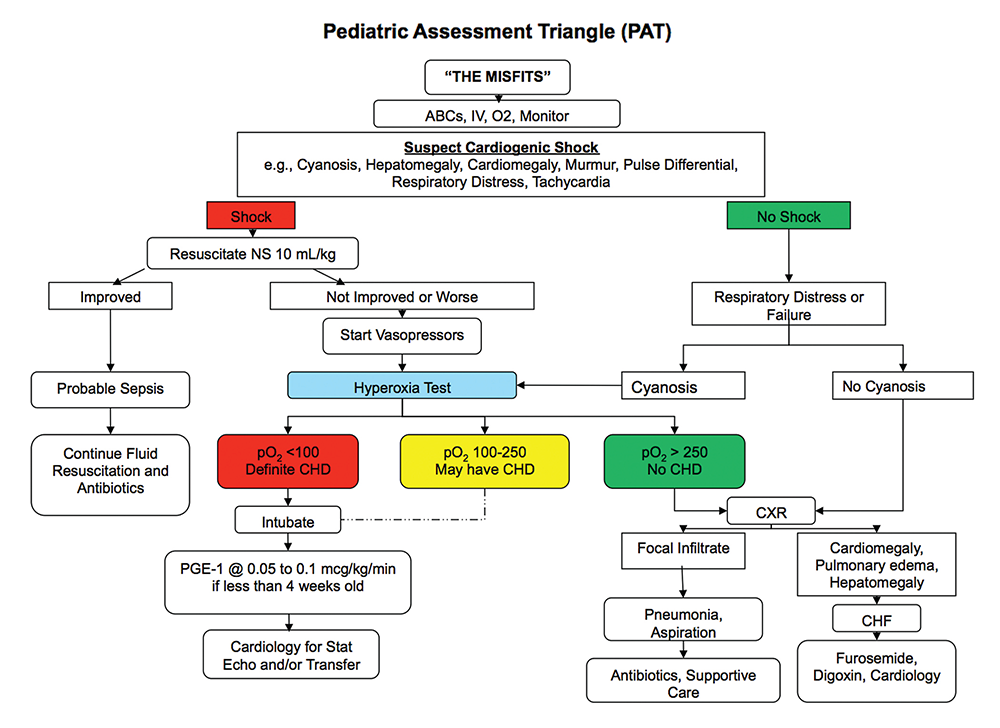
The Playbook also refers to the Pediatric Assessment Triangle (PAT), a global assessment tool that takes into account what is done in the first 20–30 seconds that you are in a patient’s room (see Figure 1). It helps to distinguish the difference between potential respiratory, cardiovascular, and metabolic etiologies of disease.
The Playbook then discusses a differential diagnosis for the sick infant: “THE MISFITS.”
T = Trauma
H = Heart disease or Hypovolemia
E = Endocrine emergencies
M = Metabolic
I = Inborn errors of metabolism
S = Seizures
F = Formula problems
I = Intestinal disasters
T = Toxins
S = Sepsis
Sepsis is deliberately saved for last as it’s common practice to treat the sick infant with antibiotics, but this encourages you not to forget other key categories of potential pathology.
The Playbook takes special time to review a specific subset of patients who will present in this age group, and those are the ones whose ductus arteriosus is closing. These patients will often present in cardiopulmonary failure, pending arrest. As the ductus closes, patients with cardiac lesions, dependent upon that route for supplemental blood flow, will decompensate. Examples of these lesions include critical coarctation of the aorta, truncus arteriosus, transposition of the great arteries, tricuspid atresia, tetralogy of Fallot, and total anomalous pulmonary venous return. To help with the diagnosis, the hyperoxia test can be performed. Place the child on a non-rebreather mask and, after several minutes, perform an arterial blood gas (ABG) test. Ideally, you obtain a preductal ABG in the right upper extremity and compare that with one on the lower extremity, but this may not be practical. In a normal circulatory system, the pO2 should be high, in the hundreds, and certainly over 250 torr. This effectively excludes congenital heart disease as an etiology. If the pO2 on supplemental oxygen is less than 100, then this is extremely predictive of hemodynamically significant congenital heart disease.
If you are giving this child 100 percent FiO2 and he doesn’t improve 100 percent—that is, his pO2 on ABG is not at least 100 torr—then he has congenital heart disease until proven otherwise. The lifesaving intervention necessary is the initiation of prostaglandins to help keep the ductus open, preserving that flow of blood. The most common side effects of prostaglandins include apnea and hypotension, so you should be prepared to address both of those conditions. See Figure 2 for a neonatal shock algorithm that incorporates these assessment tools.
“We all learned from someone who learned from someone else. We have experience spanning decades and thousands of patients,” said Dr. Horeczko. “This provides a platform for building a community together and sharing collective knowledge. I am able to provide the audience with not only the pearls and the rapid-fire information that we all crave but also with the thought process behind it. It helps to get at some of the intangibles of the practice of medicine.”
I congratulate Tim on his new endeavor and thank him for making it available to the masses. I have listened to his podcasts in the car or in the office and have taken away some very useful nuggets of information that I have already utilized. I look forward to his next installment. Give it a listen—I think you will enjoy it, too.
 Dr. Sorrentino is professor of pediatrics in the division of emergency medicine at the University of Alabama at Birmingham.
Dr. Sorrentino is professor of pediatrics in the division of emergency medicine at the University of Alabama at Birmingham.
Pages: 1 2 3 | Multi-Page






No Responses to “Pediatric Emergency Playbook Podcast a Key Resource for Emergency Physicians”