Integration of ultrasound when determining ideal needle entry in a difficult case can prevent repeated failed attempts and the overreliance on consultative services.
Explore This Issue
ACEP Now: Vol 33 – No 07 – July 2014
Ultrasound guidance is an accepted practice for many emergency medicine procedures (eg, central venous cannulation, joint aspiration, pericardiocentesis), but it is not commonly associated with benefit in lumbar punctures.1-3 Patients with nonpalpable bony landmarks and/or failed attempts can benefit from anatomical localization with ultrasound. Integration of ultrasound when determining ideal needle entry in a difficult case can prevent repeated failed attempts and the overreliance on consultative services (eg, interventional radiology or anesthesiology). A simplified two-step approach—defining the correct lumbar level and the true anatomic midline—can make this often-difficult “blind” procedure controlled and precise.
Patient Positioning
We recommend placing the patient in a sitting position, with feet supported and moderate neck flexion. The goal is to enlarge the interspinous distance; however, positioning should be determined by patient tolerance and comfort. The lateral decubitus position is also amenable to bony localization with ultrasound.
Probe Selection
The curvilinear low-frequency (5–2 MHz) transducer is ideal for imaging nonpalpable bony landmarks in the difficult adult patient. In our opinion, the linear high-frequency transducer (commonly recommended for ultrasound landmark identification) is limited in only identifying structures under 6–9 cm in depth and not ideal in a patient with a large body habitus.
Bony Landmark Identification with Ultrasound4
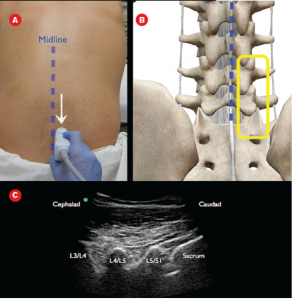
Set the ultrasound system to a depth of around 10–12 cm with presets for musculoskeletal imaging (the depth will have to be adjusted based on the patient). Position the curvilinear low-frequency transducer with probe marker cephalad near the presumed midline. Slowly slide the transducer in a lateral manner (left or right) until the facet joints are noted. A paramedian view will be obtained, allowing for imaging of the inferior and superior articular processes of the adjacent lumbar vertebrae. These facet joints will look like humps on the ultrasound screen (see Figure 1). Then slide the probe caudad until the sacrum is visualized (horizontal hyperechoic line; see Figure 2). Delineating the most inferior aspect of the lumbar spine will allow for accurate localization of the L3-L4 and L4-L5 interspaces.
From this position, slide the probe cephalad (in a paramedian plane), counting the facet joints to ensure that the initial attempt is not too caudal. Sonographers can use either the ultrasound system’s reference line or M-mode line to ensure that the center of the probe corresponds to the center of the ultrasound image. Mark the L4 and L3 facet joints (corresponding to L4-L5 and L3-L4 interspaces, respectively) on the skin surface (see Figure 3).
Rotate the transducer to the patient’s left in order to locate the true anatomic midline. Identify the bony spinous process, then slide the probe cephalad and caudad, marking the direction of the bony midline (see Figure 4). Connect the surface markings from the midline and previously identified interspace levels for an ideal location for needle entry. We recommend marking and anesthetizing two interspace levels before performing standard aseptic technique for a lumbar puncture (ensuring that the patient does not make significant movements in between skin marking and lumbar puncture needle entry). Standard lumbar puncture technique should be followed, with the clinician aware that slight needle manipulations are to be expected even though the interspace has been visualized.
Summary
Ultrasound localization for lumbar puncture can be a useful adjunct when anatomic landmarks are not palpable and/or initial attempts fail. Difficult lumbar punctures are often due to nonpalpable bony anatomy, making ultrasound localization for lumbar puncture a useful adjunct for the emergency physician.5 Errors are often due to inferior estimation of Tuffier’s line (a horizontal line connecting the top of the iliac crests that is thought to represent the L4-L5 interspace) as well as not locating the true anatomic midline.6 A simplified two-step ultrasound localization method in which the L4-L5 or L3-L4 interspace and true anatomic midline are defined can help reduce procedural error in patients with nonpalpable anatomy. The reason for ultrasound localization of bony anatomy in the difficult patient is to reduce rates of failure and reliance on consultative services.
Dr. Nagdev is director of emergency ultrasound at Alameda Health System’s Highland General Hospital in Oakland, Calif., and assistant clinical professor at the University of California, San Francisco, School of Medicine. Dr. Riguzzi and Dr. Frenkel are ultrasound fellows in the department of emergency medicine at Highland General Hospital. Dr. Mantuani is an attending physician in the department of emergency medicine and director of internal medicine point-of-care ultrasound at Highland General Hospital.
References
- Nomura JT, Leech SJ, Shenbagamurthi S, et al. A randomized controlled trial of ultrasound-assisted lumbar puncture. J Ultrasound Med. 2007;26:1341-1348.
- Peterson MA, Pisupati D, Heyming TW, et al. Ultrasound for routine lumbar puncture. Acad Emerg Med. 2014;21:130-136.
- Swaminathan A, Hom J. Does ultrasonographic imaging reduce the risk of failed lumbar puncture? Ann Emerg Med. 2014;63:33–4.
- Chin KJ, Karmakar MK, Peng P. Ultrasonography of the adult thoracic and lumbar spine for central neuraxial blockade. Anesthesiol. 2011;114:1459-1485.
- Shah KH, McGillicuddy D, Spear J, et al. Predicting difficult and traumatic lumbar punctures. Am J Emerg Med. 2007;25:608-611.
- Duniec L, Nowakowski P, Kosson D, et al. Anatomical landmarks based assessment of intravertebral space level for lumbar puncture is misleading in more than 30%. Anaesthesiol Intensive Ther. 2013;45:1-6.
Pages: 1 2 3 | Multi-Page








No Responses to “How to Perform an Ultrasound-Assisted Lumbar Puncture”