While forearm nerve blocks provide excellent anesthesia for hand injuries (fractures, dislocations, lacerations, abscesses), they don’t provide anesthesia to the volar forearm or the wrist.
Explore This Issue
ACEP Now: Vol 35 – No 10 – October 2016
Hand injuries are a very common emergency department complaint, accounting for a great deal of acute pain as well as chronic morbidity and productivity loss.1–3 Adequate analgesia and anesthesia are necessary to provide hemostasis, wound irrigation, debridement, an adequate examination, laceration or tendon repair, joint reduction, splinting, and other acute interventions. Ultrasound-guided forearm nerve blocks can provide definitive analgesia and facilitate these interventions in acute hand injuries in the emergency department.4–7

Figure 1. Distribution of the median (purpe), radial (yellow), and ulnar (red) nerves on the hand (A) and forearm (b).
Anatomy of Forearm Nerves
The distribution of nerves throughout the forearm is in three segments (see Figure 1):
- Median nerve: radial/lateral aspect of volar hand; volar surface of thumb, index, long, and radial/lateral side of ring finger
- Radial nerve: radial/lateral aspect of dorsal hand; dorsal surface of thumb; dorsal surface of index, long, and radial/lateral side of ring finger, proximal to the distal interphalangeal (DIP) joints
- Ulnar nerve: ulnar/medial aspect of dorsal and volar hand including hypothenar eminence, fifth digit, and ulnar/medial aspect of ring finger
For major injuries to the hand, such as firework blast injuries, all three forearm nerves can be blocked. For injuries to the radial aspect of the hand or the first four digits, consider blocking the median and/or radial nerve(s). For injuries to the ulnar hand or little finger (eg, a boxer’s fracture), utilize the ulnar nerve block. (See Figure 2.) There’s moderate overlap of innervation for each dermatomal location. Injuries located close to dermatomal transitions often require both nerves to be blocked to ensure adequate pain control. We also recommend using a multimodal approach to pain management that relies on oral agents as well as local anesthetic infiltration, if possible.
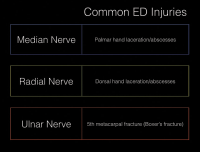
Figure 2. Choosing the correct nerve block for the injured area.
While forearm nerve blocks provide excellent anesthesia for hand injuries (fractures, dislocations, lacerations, abscesses), they don’t provide anesthesia to the volar forearm or the wrist. Therefore, other means of analgesia/anesthesia should be pursued for injuries to these areas, such as distal radius fractures and other wrist injuries.
Ultrasound Setup
Probe: The probe selection should be a high-frequency linear transducer (15-6 MHz) set at the nerve (or soft tissue) preset (found on most POCUS systems). A 10-5 MHz transducer could also be used. Use a standard 1.5-inch, 25-gauge needle. (An alternative is a 22-gauge, blunt-tipped regional block needle.)
Anesthetic: For the anesthetic, we recommend lidocaine 1 to 2 percent, bupivacaine 0.25 percent, 2 to 5 cc per nerve block. For the less experienced provider, we recommend starting with lidocaine, as bupivacaine is more commonly associated with local anesthetic systemic toxicity. All anesthetics should be used with caution when injecting near vascular structures, with LipidRescue available if needed.
Positioning: Position the ultrasound system across from the affected extremity at a comfortable height. Place the patient in a supine or 45-degree upright position, with the affected arm supinated and externally rotated and the forearm resting on a stand. As you start with the linear ultrasound probe in a transverse position in the distal forearm, align the probe marker to the same side as it appears to you on your screen. The provider should have both the ultrasound screen and the point of needle entry in the same line of sight if possible.
Locating Each Nerve
The median nerve lies along the midline of the forearm in the fascial plane between the flexor digitorum superficialis and profundus tendons. Place the linear ultrasound probe in a transverse position at the wrist crease on the volar surface of the distal forearm. Scan proximally to the mid-forearm and look for the classic “honeycomb” appearance of a nervous structure at the junction of several fascial planes (see Figure 3). There are no associated vascular structures, except in rare incidences. In the distal wrist, muscle tendon sheaths will look similar to the classic honeycomb appearance of the nerves. By scanning proximally, tendons will disappear and the nerve will be clearer.
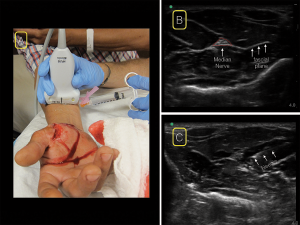
Figure 3. For the median nerve block, place the linear ultrasound probe in a transverse position at the wrist crease on the volar surface of the distal forearm. Scan proximally to the mid-forearm (A) and look for the classic “honeycomb” appearance of a nervous structure at the junction of several fascial planes (B). insert your needle from whichever side is most comfortable (A&C).

Figure 4. For the radial nerve block, starting at the wrist with the linear ultrasound probe in a transverse position over the radial artery (A), scan proximally until the nerve can be visualized separating from the radial artery (B). Locate the radial nerve between the brachioradialis and brachialis muscles. insert your needle from the radial (lateral) aspect of the probe (A&C).
The radial nerve can be found in a position radial (lateral) to the radial artery. Starting at the wrist with the linear ultrasound probe in a transverse position over the radial artery, scan proximally until the nerve can be visualized separating from the radial artery (see Figure 4). Alternatively, you can slide the probe proximally and find the nerve in the supracondylar area. Keeping the probe transverse on the lateral aspect of the arm, locate the radial nerve between the brachioradialis and brachialis muscles. You can perform the block from this position or trace the nerve back distally to a comfortable position in the forearm.
The ulnar nerve runs adjacent to the ulnar artery in the ulnar (medial) direction. Position the linear ultrasound at the wrist over the ulnar artery. Scan proximally until the nerve separates from the artery in the ulnar direction in the mid- to proximal forearm (see Figure 5). For a more comfortable position to perform an in-plane ultrasound-guided ulnar nerve block, consider having the patient abduct the arm and flex the elbow to 90 degrees, with the elbow resting on the stand.8
Performing the Block
Before your block, perform and document an appropriate neurovascular exam. After prepping the skin with antiseptic solution, use a local anesthetic to make a skin wheal at your chosen injection site. With a sterile transducer cover, insert your needle using an in-plane approach for continuous direct needle visualization. For the median nerve block, enter from whichever side is most comfortable/natural (see Figure 3). For the radial nerve block, enter the skin from the radial (lateral) aspect of the probe (see Figure 4). For the ulnar nerve block, enter from the ulnar (medial) aspect of the probe (see Figure 5).

Figure 5. For the ulnar nerve block, position the linear ultrasound at the wrist over the ulnar artery (A). Scan proximally until the nerve separates from the artery in the ulnar direction in the mid-to-proximal forearm (B). insert your needle from the ulnar (medial) aspect of the probe (A&C).
Once the needle tip is visualized to be adjacent to the nerve, slowly inject 2 to 5 mL of anesthetic into the fascial plane containing the nerve. You should see hypoechoic fluid gradually surrounding the nerve. Be careful not to insert your needle or inject anesthetic into the nerve sheath itself. Also, be careful to avoid vascular structures while inserting and removing your needle. While we recommend that novice providers use an in-plane approach for all regional nerve blocks, the median presents an opportunity to practice employing an out-of-plane approach since it doesn’t lie as close to major vascular structures as the radial and ulnar nerves.
After the Block
After performing the forearm nerve block, mark the affected extremity with the date, time, and type of block performed. Communicate with the nurse(s), other providers, and any relevant consultants that a block was performed. Of note, if consultants are to be involved in the acute care of your patient’s injury, a clear discussion regarding regional anesthesia should occur prior to performing your block. Lastly, reassess your patient to ensure adequate analgesia and assess the efficacy of your block. Be sure to reassess and document repeat neurovascular examinations.
Ultrasound-guided forearm nerve blocks are an effective method to provide analgesia for hand injuries. Because most hand injuries don’t require orthopedic consultation, we recommend that clinicians new to ultrasound-guided regional anesthesia start with ultrasound-guided forearm nerve blocks. In an era of opioid-sparing pain management, these techniques are an ideal addition to the broad armamentarium of the emergency physician.
Dr. Wroe is a senior resident at Highland Hospital, Alameda Health System, in Oakland, California.
Dr. Nagdev is director of emergency ultrasound at Highland Hospital, Alameda Health System, in Oakland, California, and assistant clinical professor at the University of California, San Francisco School of Medicine.
References
- Andrade A, Hern HG. Traumatic hand injuries: the emergency clinician’s evidence-based approach. Emerg Med Pract. 2011;13(6):1-23.
- Angermann P, Lohmann M. Injuries to the hand and wrist. A study of 50,272 injuries. J Hand Surg Br. 1993;18(5):642-644.
- de Putter CE, van Beeck EF, Polinder S, et al. Healthcare costs and productivity costs of hand and wrist injuries by external cause: a population-based study in working-age adults in the period 2008-2012. Injury. 2006;47(7):1478-1482.
- Liebmann O, Price D, Mills C, et al. Feasibility of forearm ultrasonography-guided nerve blocks of the radial, ulnar, and median nerves for hand procedures in the emergency department. Ann Emerg Med. 2006;48(5):558-562.
- Frenkel O, Liebmann O, Fischer JW. Ultrasound-guided forearm nerve blocks in kids: a novel method for pain control in the treatment of hand-injured pediatric patients in the emergency department. Pediatr Emerg Care. 2015;31(4):255-259.
- Sohoni A, Nagdev A, Takhar S, et al. Forearm ultrasound-guided nerve blocks vs landmark-based wrist blocks for hand anesthesia in healthy volunteers. Am J Emerg Med. 2016;34(4):730-734.
- Wroe P, O’Shea R, Johnson B, et al. Ultrasound-guided forearm nerve blocks for hand blast injuries: case series and multidisciplinary protocol. Am J Emerg Med. 2016;34(9):1895-1897.
- Toles K, Nagdev A. Trick of the trade: patient positioning for ultrasound-guided ulnar nerve block. Academic Life in Emergency Medicine website. Accessed Sept. 14, 2016.
Pages: 1 2 3 4 | Multi-Page





No Responses to “How to Perform Ultrasound-Guided Forearm Nerve Blocks to Provide Non-Drug Pain Relief for Acute Injuries”