Explore This Issue
ACEP Now: Vol 33 – No 08 – August 2014Understanding POLST forms will better enable emergency physicians to verify patients’ wishes for end-of-life care are being met
As the front line in care, emergency physicians often approach a patient in extremis or with a dramatic change in clinical condition. We may be presented with a Physician Orders for Life-Sustaining Treatment (POLST) form for a patient who has limited or no ability to communicate. Some background and cases will illustrate relevant considerations.1
What Is POLST?
The POLST form is part of a program to foster communication and shared decision making about goals of care at the end of life. The conversation is to occur between the patient or surrogate and a health care professional when the patient is diagnosed with a serious illness or frailty where the provider “would not be surprised if the patient died within the next year,” an outcome that is difficult to predict precisely.2,3 The health care professional documents the patient’s preferences as medical orders when the POLST form is completed.
Forty-three states currently have a fully endorsed or developing POLST program that is designed along the paradigm with shared core principles and similar form design.4 States may differ, however, in the terminology (eg, POLST, Physician Orders for Scope of Treatment [POST], Medical Orders for Life-Sustaining Treatment [MOLST], Medical Orders for Scope of Treatment [MOST]); color of the form (eg, bright pink, green, white, or copies); which health care professional is authorized to sign (eg, physician, nurse practitioner, physician assistant); whether the patient or surrogate must sign; action prompted by a blank section of the form; whether the program is delineated in statute, in regulation, or by a consensus panel; how to address a conflict between a POLST form and an advance directive; the degree of immunity; duty to comply; and the level of reciprocity with other states’ POLST programs. To understand many states’ specifics, visit the National POLST Paradigm’s website at www.polst.org.
Details of the POLST Form
Not all POLST forms are identical. The POLST form (see Figure 1) should include the patient’s name and authorized signatures of the health care provider and patient or surrogate. The top section, with a selection regarding resuscitation, applies if the patient is in cardiac arrest. The next sections usually describe goals of treatment, level of medical interventions, antibiotics, artificially administered hydration, and nutrition. The lower portion includes discussion of care goals.
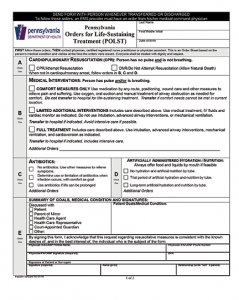
Figure 1. POLST form for Pennsylvania, available at http://www.polst.org/educational_resource/pennsylvania-polst-form.
A patient’s POLST form should be readily accessible by caregivers and EMS to facilitate its implementation. The form should accompany the patient on transfer. In states with POLST programs, most hospitals honor the POLST form that accompanies a patient until the patient is reassessed. In an emergency where the attending physician is precluded from discussion with the patient, the orders expressed on the POLST form should be followed. Challenges include when the POLST form is unavailable, incomplete, unsigned, or with a seeming inherent contradiction (eg, DNR/full treatment, attempt cardiopulmonary resuscitation, and comfort measures only).5,6
How Does a POLST Form Differ From an Advance Directive?
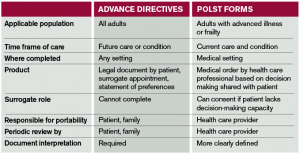
The POLST form complements an advance directive (see Table 1). It is not necessarily a request to withhold resuscitation. In the prehospital setting, POLST expands out-of-hospital DNR orders, which only apply when the patient is in cardiopulmonary arrest.
Case 1: A 55-year-old male with aggressive lymphoma responding well to treatment is visiting from out of state. He presents to the ED with cough, fever, rigors, and dyspnea. He develops hypotension, hypoxemia, and increased respiratory distress but retains decision-making capacity. He brings his POLST form completed in his home state that states, “Do Not Attempt Resuscitation and Limited Additional Interventions (which excludes mechanical ventilation).” You discuss with him whether he would reconsider and be intubated. He consents to intubation, and you proceed accordingly.
The patient with decision-making capacity has authority to override a prior POLST order. It is essential whenever possible to pause and review with the patient or surrogate to assess if they want to change their request from what is on the POLST form. This patient’s expressed decision (or, in another case, confirmation) makes moot the question of whether the form is valid outside the jurisdiction in which it was created.
Case 2: An 82-year-old female with a history of congestive heart failure presents with new onset confusion and a headache. CT shows a large intracerebral hemorrhage, which causes her to lose her decision-making capacity and from which she is not expected to recover. She is accompanied by her health care surrogate and a POLST form that indicates the patient wants CPR. The surrogate points to a notation that the form was completed when the patient had hoped to attend her great-granddaughter’s wedding, which has now already occurred. The POLST form is revised to reflect the new health condition and advise DNR, comfort measures only, and she receives palliative care.
This highlights the surrogate’s instrumental role in ensuring the goals of the patient are implemented. While there may be instances where the view of the surrogate and the intent of the patient differ, each state can establish safeguards to help ensure that the surrogate carries out the patient’s wishes. Such steps may require that a surrogate consult with the treating physician before authorizing a change to the patient’s POLST form, that the patient’s advance directive is reviewed, that good-faith efforts are made to act consistently with the patient’s known wishes, and that the reason for a change in the patient’s POLST is carefully documented.
Do we have legal protection? Emergency physicians are generally reassured by statutory immunity associated with a state’s laws on advance directives and surrogates. In states without a similar level of explicit immunity from criminal prosecution, civil liability, and disciplinary sanctions when POLST orders are followed in good faith, the liability climate may influence the acceptance of POLST orders.7 It is important to familiarize yourself with the protections in your state.
As POLST programs become more established in communities, emergency physicians are increasingly likely to care for patients with POLST forms. Better understanding of these programs may enhance the end-of-life care we provide.
References
- POLST Legislative Guide. National POLST Paradigm Web site. Available at: http://www.polst.org/wp-content/uploads/2014/02/2014-02-20-POLST-Legislative-Guide-FINAL.pdf. Accessed June 2, 2014.
- Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the “surprise” question in cancer patients. J Palliat Med. 2010;13:837-40.
- Moss AH, Ganjoo J, Sharma S, et al. Utility of the “surprise” question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol. 2008;3:1379-84.
- POLST Programs in Your State. National POLST Paradigm Web site. Available at: http://www.polst.org/programs-in-your-state/. Accessed June 2, 2014.
- Schmidt TA, Zive D, Fromme EK, et al. Physician orders for life-sustaining treatment (POLST): Lessons learned from analysis of the Oregon POLST Registry. Resuscitation. 2014;85:480-5. Jesus JE, Geiderman JM, Venkat A, et al.
- Physician orders for life-sustaining treatment and emergency medicine: Ethical considerations, legal issues, and emerging trends. Ann Emerg Med. 2014;pii:S0196-0644(14)00220-0.
- Statutory/Regulatory Comparison of State POLST Programs, January 2013: ABA Commission on Law and Aging. National POLST Paradigm Web site. Available at: http://www.polst.org/wp-content/uploads/2013/05/Leg-Chart-POLST_3-21-13-AG.pdf. Accessed June 2, 2014.
Dr. Heine practices emergency medicine and hematology oncology in Pennsylvania.
Pages: 1 2 3 | Multi-Page





No Responses to “Physician Orders for Life-Sustaining Treatment Forms: What You Need to Know”