
Texas Health Harris Methodist Hospital Fort Worth is part of a 25-hospital system and one of the busiest emergency departments in the country. With 635 inpatient beds, the hospital houses a 100-bed ED, which treated approximately 120,000 patients last year. Its admission rate is high at 24 percent, and it has a high ambulance arrival rate of 30 percent. The ED leadership and staff moved into their new facility approximately two years ago, and it boasts five zones and 75,000 square feet. Even before moving to the new facility (the old one was only a third of the size), the department had a reputation for service quality and efficiency.
Explore This Issue
ACEP Now: Vol 35 – No 03 – March 2016The Texas Health Fort Worth ED has unrivaled performance in both clinical and operational metrics. Most of its core measure metrics (pneumonia, stroke, ST elevation myocardial infarction, sepsis) had performance above 95 percent, with many at 100 percent. Further, its operational performance is unheard of in EDs seeing more than 100,000 patients a year:
- Door-to-doctor time is 20 minutes.
- Overall length of stay is 185 minutes.
- Length of stay of admitted patients is 291 minutes.
What are some of its strategies for such outstanding workflow, patient flow, and clinical quality? This department is staffed by an extremely stable physician group with strong leadership and a long history of service quality. The ED group was founded and led by John Geesbreght, MD, FACEP, who was formerly in the military and is, by all accounts, a visionary and a gifted operational thinker. He was joined early on by Elliott Trotter, MD, and Ralph Baine, MD (who was a nurse when he initially joined the group), who shared his vision for an efficient and patient-centric emergency medicine practice. Interestingly, Texas Health Fort Worth has some half a dozen physicians who came up through the ranks as nurses or scribes and then returned to the group after completing medical training.
Physicians … move from the highest-acuity area to the lowest-acuity area during a shift.
Dr. Geesbreght and his leadership team have designed one of the most unique and original physician-staffing models in use. Despite promoting individual physician efficiency, this physician group recognizes that there are fast physicians and slow physicians. Though the group tracks efficiency metrics on all physicians and inspires them to work as efficiently as possible, it realizes that there are intrinsic differences. Doctors are monitored for productivity and classified as green, yellow, or red, indicating the highest to lowest productivity, respectively. This is not used in a punitive fashion because this group recognizes that each physician member contributes to the good of the group in some way: some are researchers, some are teachers, some are IT experts, and some play a role in the EMS community, etc. However, when the clinical schedule is crafted, there is careful effort not to schedule consecutive or concurrent red physicians.
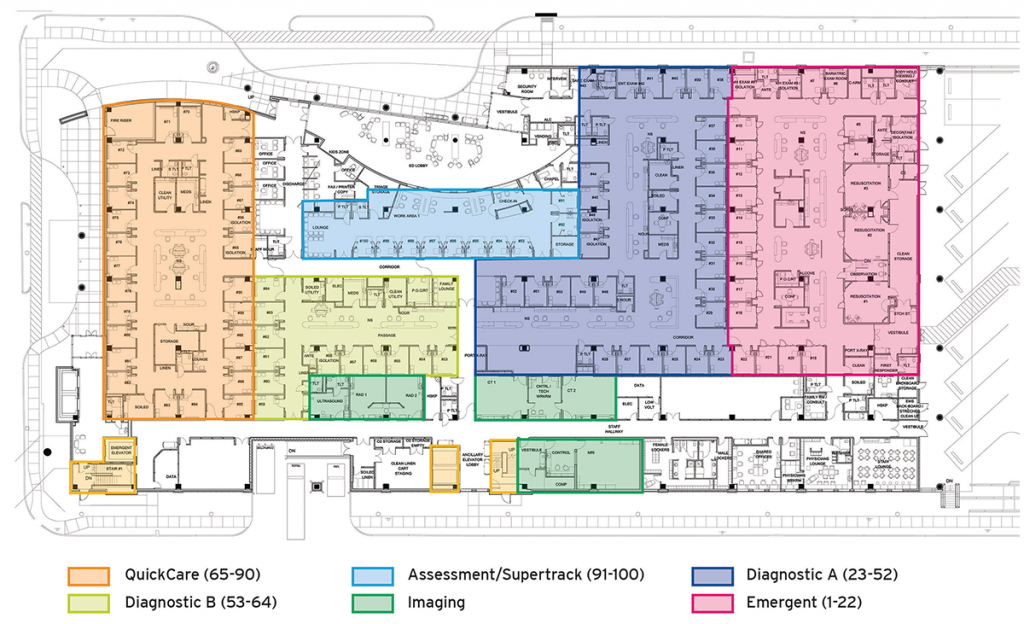
The ED at Texas Health Fort Worth was designed as an I-beam configuration, with five zones that care for patients based on triage acuity (see Figure 1). The most recently arrived physician treats the sickest, least stable patients in the critical care area.
Physicians progress through a schedule that has them move from the highest-acuity area to the lowest-acuity area (Critical Care –> Medical A & B –> Quick Care) during a shift. Procedures are handed off to a procedure physician who only does procedures. This will probably be the most controversial aspect of this scheduling paradigm, but it’s explained by Terence McCarthy, MD, in a way that every emergency physician understands. If you’re intensely involved with a patient who may be septic but you also have a three-layer facial laceration to close and are interrupted and distracted, you may feel afterward that you did not do your best. Imagine if all you had on your plate were procedures done in series. Since every physician works through the progression, every physician has the opportunity to perform procedures. The model is also noteworthy for placing the most rested physicians in the area with the most clinically complex and ill patients. The shift finishes in the minor care area, which excludes patients with abnormal vital signs. Physicians are encouraged to make efficient and rapid dispositions of these patients because if they are unable to tidy up a zone as they progress through it, then they may have active patient care going on over a large ED footprint. The physicians admitted that, on occasion, the geography and the physician-progression model seem at odds and a physician is doing a lot of running, but the doctors explained that their model had many advantages viewed as, “what is good for the patients.”
The proof of physician satisfaction is in the retention pudding. Texas Health Fort Worth has very low staff turnover. When asked about the last time a physician left the group, Richard Dixon, MD, and Dr. McCarthy scratched their heads. “Remember in 2002?” Both physicians and nurses are screened for a high work ethic and standard and good teamwork skills. The glue that seems to hold it all together is a genuine commitment to the patient.
This innovative model for staffing and the delivery of patient care goes against the conventional wisdom of med teams in a geographic zone, but it clearly works. That said, it requires a high level of teamwork and collaboration, a culture of putting patients first, and a commitment to continuous improvement. If you have all of this going for you, this is a care-delivery model that is worth exploring.
Hats off to the ED at Texas Health Fort Worth. It is living proof of what a well-run ED can accomplish!
Pages: 1 2 3 | Multi-Page





No Responses to “Physician Staffing Model at Texas Health ED Helps Maintain Top Clinical, Operational Metrics”