The Case
A 6-year-old girl presents to the emergency department after waking up at midnight with another asthma exacerbation. She had been getting worse despite using her albuterol correctly. After receiving three treatments with albuterol and Atrovent, she is doing much better. You prepare to discharge her on a three-day course of prednisolone (PRED). Her parents ask if there is something else that tastes better because it is a real struggle to get her to take the medicine.
Explore This Issue
ACEP Now: Vol 37 – No 02 – February 2018Background
PRED has been the oral steroid used in the treatment of pediatric asthma exacerbations for decades. However, it has a bitter taste that can make it very hard to administer to a young child. PRED is also associated with a significant amount of vomiting; this is one of the leading reasons for treatment failure for outpatient asthma.1
Dexamethasone (DEX) has a longer half-life than PRED, is much better tolerated, and has been used for a variety of pediatric conditions, including croup.2,3 A number of recent studies have compared PRED to DEX for the outpatient treatment of asthma. A systematic review and meta-analysis showed that a single- or two-dose regimen of DEX was as effective as a five-day course of prednisone/PRED, with less vomiting in the DEX group.4
All the studies have shown that DEX was as good as PRED for the treatment of asthma. Of the seven randomized control trials, all have issues with methodology and utilized different doses.
Clinical Question
In children presenting to the emergency department with an acute exacerbation of asthma, is a single oral dose of DEX noninferior to three days of PRED?
Reference
Cronin JJ, McCoy S, Kennedy U, et al. A randomized trial of single-dose oral dexamethasone versus multidose prednisolone for acute exacerbations of asthma in children who attend the emergency department. Ann Emerg Med. 2016;67(5):593-601.e3.
- Population: Patients between 2 and 16 years of age with a prior history of asthma presenting to the emergency department with an acute asthma exacerbation.
- Excluded: Anyone with a critical or life-threatening exacerbation, varicella or herpes simplex virus infection, tuberculosis exposure, fevers higher than 39.5ºC, steroid use within the last four weeks, metabolic disease, or any comorbid condition.
- Intervention: DEX 0.3 mg/kg (maximum 12 mg) orally once.
- Comparison: PRED 1 mg/kg per day (maximum 40 mg/day) orally for three days.
- Outcomes:
- Primary: Pediatric Respiratory Assessment Measure (PRAM; range 0 to 12) at day four of treatment (see Table 1).
- Secondary: Change in PRAM score, PRAM score at emergency department discharge, hospital admission on day one, emergency department length of stay, unscheduled visits to health care providers for respiratory symptoms, readmission to the hospital or additional systemic corticosteroids within 14 days of study enrollment, vomiting within 30 minutes of administration of the study medication, school days and parental workdays missed, and days of restricted activity.
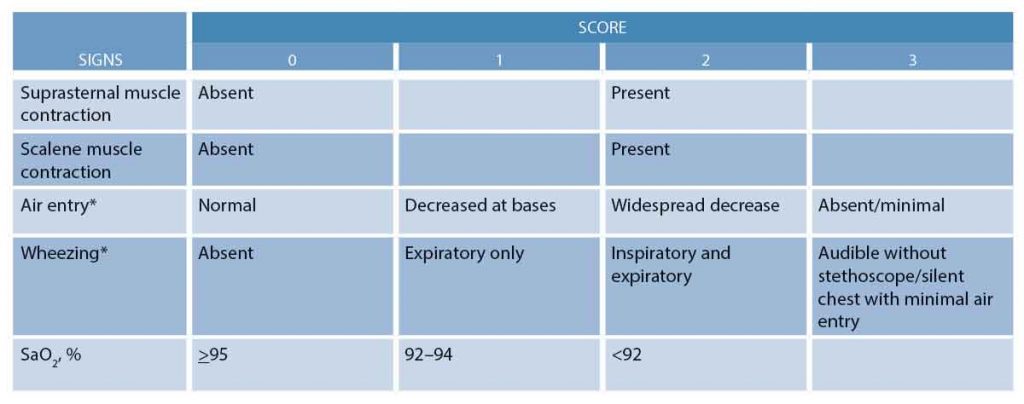
(click for larger image) Table 1. The Pediatric Respiratory Assessment Measure (PRAM)
*In case of asymmetry, the worst lung is rated. Mild exacerbation=1 to 3; moderate, 4 to 7; and severe, 8 to 12.
Source: Cronin JJ, McCoy S, Kennedy U, et al. A randomized trial of single-dose dexamethasone versus multidose prednisolone for acute exacerbations of asthma in children who attend the emergency department. Ann Emerg Med. 2016;67(5):593-601.e3.
Authors’ Conclusion
“In children with acute exacerbations of asthma, a single dose of oral dexamethasone (0.3 mg/kg) is noninferior to a 3-day course of oral prednisolone (1 mg/kg per day) as measured by the mean PRAM score on day 4.”
Key Results
There were 226 children included in this study, with more boys than girls. The mean age was around 6 years.
- Primary Outcome: There was no difference in mean PRAM scores at day four between the DEX and PRED groups.
- Mean PRAM 0.91 DEX versus 0.91 PRED (95% CI, -0.35 to 0.34)
- Secondary Outcomes:
- There was no difference between groups for any of the secondary outcomes except for further systemic steroids (13.1 percent DEX versus 4.2 percent PRED).
- Fourteen patients in the PRED group vomited, while no patients in the DEX group vomited.
Evidence-Based Medicine Commentary
- Blinding: This was not a blinded study, which could have introduced bias. It would have been better if the participants and providers did not know what treatment was being received.
- Selection Bias: Some of the exclusion criteria were subjective in nature. This could have introduced bias into the study.
- Prognostic Factors: In the DEX group, there were higher rates of atopic dermatitis, stronger family histories for both atopic dermatitis and asthma, and higher rates of daily usage of salbutamol. This might indicate that the DEX group was sicker than the PRED group. This imbalance of prognostic factors could have skewed the data to make them less significant when compared with the PRED group.
- Side Effects: Vomiting was the most common side effect but was not observed in the DEX group. A common reason to fail outpatient management is not being able to tolerate oral medications (vomiting). The lack of vomiting in the DEX group would bias the results away from oral PRED.
- Treatment Failure: The DEX group had a higher number of treatment failures that required a second course of steroids. However, these patients were older and, based on their PRAM scores, were actually sicker than the other patients in the study. This observation also held true for the PRED group. A possible reason for treatment failure is that providers in the United Kingdom and Ireland use a lower dose of DEX (0.3 mg/kg) than those in the United States (0.6 mg/kg). However, similar failure rates have been observed in other studies done in the United States using the higher-dosing regimen. What some clinicians do is provide a second dose of DEX for the sicker child to take 48 hours postdischarge.
Bottom Line: In children presenting to the emergency department with an acute exacerbation of asthma, a single dose of DEX is noninferior to a three-day course of oral PRED.
Case Resolution
The 6-year-old girl who did not like the taste of PRED was given oral DEX 0.6 mg/kg. A second dose was provided to be given if needed at 48 hours.
Thank you to Dr. Michael Falk, a pediatric emergency medicine provider working at Harlem Hospital Center in New York and Children’s National Medical Center in Washington, D.C. He is also a Best Evidence in Emergency Medicine (BEEM) presenter and author.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
References
- Lucas-Bouwman ME, Roorda RJ, Jansman FG, et al. Crushed prednisolone tablets or oral solution for acute asthma? Arch Dis Child. 2001;84(4):347-348.
- Schimmer BP, Parker KL. Adrenocorticotropic hormone; adrenocortical steroids and their synthetic analogs; inhibitors of the synthesis and actions of adrenocortical hormones. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 11th ed. New York: McGraw-Hill; 2007:1587-1612.
- Russell KF, Liang Y, O’Gorman K, et al. Glucocorticoids for croup. Cochrane Database Syst Rev. 2011;(1):CD001955.
- Keeney GE, Gray MP, Morrison AK, et al. Dexamethasone for acute asthma exacerbations in children: a meta-analysis. Pediatrics. 2014;133(3):493-499.
Pages: 1 2 | Multi-Page






One Response to “Prednisolone or Dexamethasone for Pediatric Asthma Exacerbations?”
March 4, 2018
GaryThe IV formation of dexamethasone, which is commonly used po, is slightly less absorbed from the gi tract, so I would lean towards giving the higher dose seen in other studies of 0.6mg/kg to a max of 16mg, which is also a protocol used at many US children’s hospitals.