Have you wondered why a particular patient coded after endotracheal intubation? Actually, it is not uncommon for critically ill patients to decompensate during or after this essential intervention. While approximately 60 percent of critically ill patients require endotracheal intubation,1 it also puts them at high risk for hemodynamic collapse during the procedure. Prior studies suggest that there is up to a 25 percent risk of hemodynamic instability even in successful critical care unit intubations.2 Therefore, hemodynamic optimization is crucial prior to endotracheal intubation to prevent peri-intubation hemodynamic instability and poor patient outcomes.
Explore This Issue
ACEP Now: Vol 41 – No 02 – February 2022Heart Failure Considerations
Endotracheal intubation is especially perilous for a patient with right ventricular (RV) failure, which can occur because of abruptly increased RV afterload or decreased contractility from a wide range of clinical conditions, including pulmonary embolism, acute exacerbation of chronic lung disease, or acute respiratory distress syndrome.3,4 RV failure is an underdiagnosed condition in patients undergoing intubation and invasive mechanical ventilation. Performing this procedure in patients with RV failure can result in catastrophic hemodynamic collapse because the failing right heart is very sensitive and unable to compensate for any increase in afterload and/or decrease in preload from intubation.
The normal right ventricle is thin-walled, highly compliant, and typically ejects blood against a vascular resistance only 20 percent that of the systemic circulation. Even a slight increase in pulmonary vascular resistance can overload a normal right ventricle, and it does not handle increases in afterload well under conditions such as pulmonary embolism, resulting in RV dilatation and, when severe, RV failure. As RV failure progresses, the interventricular septum bulges to the left, compresses the left ventricular cavity, impairs filling of the left ventricle, and reduces the septal contribution to RV contractility. This left-sided septal shift leads to reduced cardiac output and systemic hypotension. The effects of intubation and invasive mechanical ventilation will exacerbate this situation, resulting in hemodynamic collapse and, in some cases, cardiac arrest.5
Point-of-care echocardiography has evolved as a simple, portable, and rapid noninvasive tool for assessment of hemodynamic status. It provides invaluable information for diagnoses and direct resuscitation in critically ill patients, including assisting in the evaluation of intravascular volume status and fluid responsiveness. This bedside imaging modality can help guide appropriate interventions prior to patient decompensation and assess responses to interventions. Preintubation echocardiography allows for direct and noninvasive visualization of the right ventricle at the bedside and can play a major role in the hemodynamic stabilization of critically ill patients. It allows clinicians to implement therapeutic strategies to prevent potential hemodynamic decompensation during and following endotracheal intubation in patients with RV failure. Preintubation echocardiography can detect signs of RV failure (pressure and volume overload) such as right ventricle dilation (best appreciated in the four-chamber view), septal flattening visualized as “D-sign” and bowing of the interventricular septum into the left ventricle on a parasternal short-axis view, decrease in the size of left ventricular cavity, and decreased left ventricular filling leading to decreased cardiac output (Figures 1–3).4 With detection of echocardiographic signs of RV failure, different ameliorating strategies can be employed prior to intubation to optimize hemodynamics and avoid worsening RV failure and cardiovascular collapse. Sonographic assessment allows clinicians to approach preintubation resuscitation in a specific, targeted manner that includes volume optimization, restoration of perfusion pressure, and improvement of myocardial contractility.
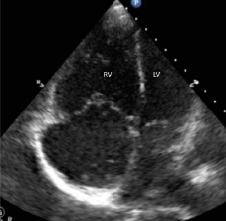
Figure 1: Four-chamber apical view demonstrating enlarged right ventricle (RV).
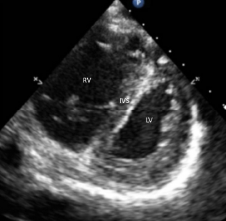
Figure 2: Bowing of the interventricular septum (IVS) into left ventricle is visualized as “D-sign” on a parasternal short-axis view in a patient with right ventricular (RV) failure.
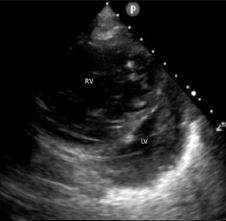
Figure 3: Parasternal short-axis view showing decrease in the size of left ventricular (LV) cavity.
Endotracheal intubation should be avoided or delayed when possible as this is an extremely high-risk procedure in patients with RV failure. If the intubation is unavoidable, avoid excess positive end-expiratory pressure (PEEP) or airway pressures. An alternative in some cases is noninvasive positive pressure ventilation, which has a less pronounced effect on venous return and preload compared to invasive mechanical ventilation. A common misconception is that RV failure should consistently be treated with volume supplementation. In a large proportion of cases, RV failure is associated with excessive preload. In such cases, volume resuscitation can overdistend the RV and thereby increase RV wall stress, decrease contractility, increase interventricular dependence, reduce left ventricular filling, and ultimately decrease cardiac output. Unlike other causes of shock, fluid boluses can actually worsen hemodynamics in RV failure and generally should not be administered in RV failure patients during the peri-intubation period. In the setting of acute RV failure due to pulmonary embolism, an inhaled pulmonary vasodilator, such as nitric oxide, can be used for afterload optimization in the peri-intubation period to decrease pulmonary artery pressure through pulmonary vasodilation.
How to Avoid Making the Worst of a Bad Situation
With the exception of patients with severe left ventricular failure, pulmonary vasodilators offer numerous benefits, including improved oxygenation and ventilation (due to facilitation of ventilation-perfusion matching) and decreased pulmonary vascular resistance without causing systemic hypotension. Another strategy to avoid worsening RV failure includes the administration of vasopressors (epinephrine, vasopressin, or norepinephrine) prior to endotracheal intubation while avoiding phenylephrine. In a hypotensive patient with severely elevated pulmonary artery pressure, vasopressors can raise systemic arterial pressure, augment cardiac output, and reduce the risk of exacerbating RV ischemia.6
The failing right ventricle is exquisitely sensitive to changes in preload, afterload, and contractility in the peri-intubation period. Identification of acute RV failure and careful hemodynamic optimization are crucial to improve outcomes in patients undergoing endotracheal intubation. The complexity of hemodynamic management in acute RV failure creates a powerful argument for emergency physicians to use preintubation echocardiography. With increasing use of point-of-care ultrasound, emergency physicians are well-positioned to use echocardiography for hemodynamic optimization prior to intubation. It can provide invaluable information regarding RV structure and function, help guide interventions, and improve safety in critically ill patients.
Dr. Adhikari is a tenured Professor, Chief of Emergency Ultrasound section and Emergency Ultrasound Fellowship Director at the University of Arizona in Tucson, Arizona.
References
- Smischney N, Kashyap R, Seisa M, et al. Endotracheal intubation among the critically ill: protocol for a multicenter, observational, prospective study. JMIR Res Protoc. 2018;7(12):e11101.
- Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120(2):323-352.
- Ahmed A, Azim A. Difficult tracheal intubation in critically ill. J Intensive Care. 2018;6:49.
- Krishnan S, Schmidt GA. Acute right ventricular dysfunction: real-time management with echocardiography. Chest. 2015;147(3):835-846.
- Arrigo M, Huber LC, Winnik S, et al. Right ventricular failure: pathophysiology, diagnosis and treatment. Card Fail Rev. 2019;5(3):140-146.
- Konstam MA, Kiernan MS, Bernstein D, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation. 2018;137(20):e578-e622.
Pages: 1 2 | Multi-Page




No Responses to “Preintubation Point-of-Care Echocardiography for Hemodynamic Optimization”