Once upon a time, the emergency department was a single treatment room in the basement of a hospital. As utilization grew, the footprint of the ED grew, and by the 1980s, most EDs consisted of many rooms creating an entire department for urgent and emergent care. Emergency physicians discovered that patients with minor injuries could be treated and separated from the main department. With the right resources, patients could be treated and released in a more efficient manner by creating the “Fast Track” for high census times of the day. In the 1990s, emergency physicians at higher-volume centers found that some patients needed 24 hours to be adequately diagnosed and treated; the heyday for the ED observation unit began. These innovations were the tip of the iceberg, and performance-driven emergency departments have been experimenting with an array of models that segment patients into patient streams for more efficient health care delivery.1–3 The Supertrack (for very-low-acuity patients needing no resources), the pediatric ED, the geriatric ED, the CDU (clinical decision unit), and chest pain units are examples of patient segmentation currently employed across the country.
Explore This Issue
ACEP Now: Vol 34 – No 11 – November 2015The Raritan Bay Medical Center emergency department, with the support of Vincent Ciccarelli, MBA, BSN, ED nurse director, reinvented its intake process to quickly segment patients into appropriate areas within the department.
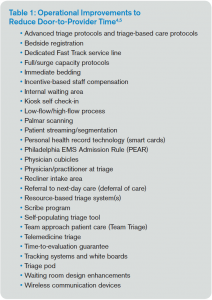
It is a fact: the world is watching the fishbowl that is the emergency department. Consumers, payers, and practitioners are intensely studying the Centers for Medicare & Medicaid Services’ emergency medicine performance metrics like OP-18 and ED-1a, capturing the length of stay of discharged and admitted patients, respectively. Also receiving attention is OP-20, the time from arrival to evaluation by a qualified medical provider. Here, too, we find a number of operational improvements emerging that improve the time it takes to see a provider (see Table 1).4,5
This month’s column will focus on a real success story from an ED trying to improve its front-end operations. Geralda Xavier, MD, MPH, the medical director at Raritan Bay Medical Center in Perth Amboy, New Jersey, wanted to improve the intake process for the emergency department. She found what other medium- and high-volume EDs have discovered. They are having success and gaining efficiency by quickly assigning patients to different streams based on specific criteria. The Raritan Bay Medical Center emergency department, with the support of Vincent Ciccarelli, MBA, BSN, ED nurse director, reinvented its intake process to quickly segment patients into appropriate areas within the department. This expedited the time to see the physician or other provider.
The characteristics of the Raritan Bay ED are outlined below:
Perth Amboy
Beds – 36
Annual volume – 47,000
Admissions – 17%
Length of stay discharged – 227 minutes
Left without being seen – 3.2%
As with most EDs, the most difficult process involved the appropriate segmentation of Emergency Severity Index (ESI) 3 patients. Most EDs triage nearly half of their patients into this group, and it encompasses a vast array of chief complaints and acuities. The Perth Amboy ESI distribution follows:
ESI Distribution
ESI 1 – 0.4%
ESI 2 – 11%
ESI 3 – 43%
ESI 4 – 33%
ESI 5 – 7%
The Raritan Bay improvement team came up with a segmentation scheme that allowed some ESI 3 patients to remain vertical while others were placed in beds. The guidelines for the ESI 3 vertical and ESI 3 horizontal patients are in Table 2.
Patients arriving were quickly seen by a “pivot nurse.” A pivot nurse is an experienced nurse with extra training in assigning patients to the segmentation model. The patients with triage acuity 1 or 2 or horizontal 3 went to one area, the patients with ESI indices of 4 and 5 and vertical 3 made up another stream. Patients were then quickly seen by a provider. Patients went to the area in the department with the appropriate resources for that patient.
Results:
Door-to-Doctor Time
BEFORE 45 minutes
AFTER 28 minutes
The Perth Amboy ED team has a great success story to tell. But even more, they have given ED practitioners a model to experiment with for the patient segmentation and streaming of ESI 3 patients, our biggest and most diverse bucket of patients. This is cutting-edge ED operations. Bring it on!
References
- Jensen K, Crane J. Improving patient flow in the emergency department. Healthc Fincanc Manage. 2008;62(11):104-106, 108.
- Ieraci S, Digiusto E, Sonntag P, et al. Streaming by case complexity: evaluation of a model for emergency department Fast Track. Emerg Med Australas. 2008;20(3):241-249.
- Kinsman L, Champion R, Lee G, et al. Assessing the impact of streaming in a regional emergency department. Emerg Med Australas. 2008;20(3):221-227.
- Wiler J, Gentle C, Halfpenny J, et al. Optimizing emergency department front-end operations. Ann Emerg Med. 2010;55(2):142-160.
- Welch S, Savitz L. Exploring strategies to improve emergency department intake. J Emerg Med. 2012;43(1):149-158.
Pages: 1 2 | Multi-Page






No Responses to “Segmentation Improves Emergency Department Patient Flow at Raritan Bay Medical Center”