
1.All Superficial Venous Thromboses Are Created Equal?
Explore This Issue
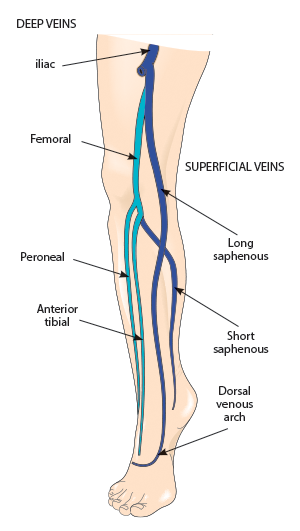
ACEP Now: Vol 36 – No 01 – January 2017Figure 1: Deep and superficial veins
Credit: SHUTTERSTOCK.COM
It is very easy to take the ultrasound report at face value and treat superficial venous thrombosis (SVT) as a benign entity distinctly different from deep venous thrombosis (DVT). However, that reasoning may result in missed or delayed diagnosis of DVT or inadequate treatment of at-risk patients. The belief that SVT is benign and DVT is potentially serious is an oversimplification of the disease process. The fact is that venous thrombosis is a continuum, and SVT and DVT are directly linked and not distinctly different. The key is in the location of the clot and the patient’s risk profile. Emergency physicians, and patients, can be victimized by limited data on an ultrasound report. All SVTs are not created equal. It’s just like real estate—location, location, location.
In an enlightening review article, Litzendorf and Satiani report that the incidence of DVT from SVT ranges from 6 percent to 40 percent (those with a history of prior DVT) and that the incidence of symptomatic pulmonary embolism (PE) associated with SVT ranges from 2 percent to 13 percent.1 In short, an isolated distal lesser saphenous vein SVT is not the same as one at or approaching the saphenopopliteal junction or, worse, the saphenofemoral junction (see Figure 1). Despite the usual limitations of a review article, it provides some nice insight into recognition of those at risk for clot propagation and development of DVT or even PE. Nonsteroidal anti-inflammatory drugs and heat are probably fine for inconsequential SVTs. However, systemic anticoagulation (just like a DVT), repeat ultrasound to look for propagation, and investigation of risk factors (eg, prior DVT, a history of malignancy, the presence of varicosities, and hypercoagulable disorders [up to 35 percent of patients with SVT]) are important considerations with a precariously placed proximal SVT. This article provided a nice flowchart (see Figure 2), prompting treatment options based on several factors. Concomitant DVT is also common. Binder et al, in a prospective, observational study, noted that in 46 consecutive patients with SVT, 24 percent had concomitant DVT, with 73 percent in the affected leg, 9 percent in the contralateral leg, and 18 percent in both legs.2
There is no single right answer because so many variables may impact the treatment plan. However, recognizing the significance of proximal SVT, compared to other locations, and considering concomitant DVT are critical to ensuring a good outcome.
Pages: 1 2 3 4 | Single Page






No Responses to “Superficial Venous Thromboses, Intracranial Aneurysms, and Treating High Glucose Levels: More Myths in Emergency Medicine”